
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
- Efficacy and Safety of IDegAsp in a Real-World Korean Population with Type 2 Diabetes Mellitus
- Shinae Kang, Yu-Bae Ahn, Tae Keun Oh, Won-Young Lee, Sung Wan Chun, Boram Bae, Amine Dahaoui, Jin Sook Jeong, Sungeun Jung, Hak Chul Jang
- Received August 24, 2023 Accepted November 22, 2023 Published online February 27, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0297 [Epub ahead of print]
- 646 View
- 42 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
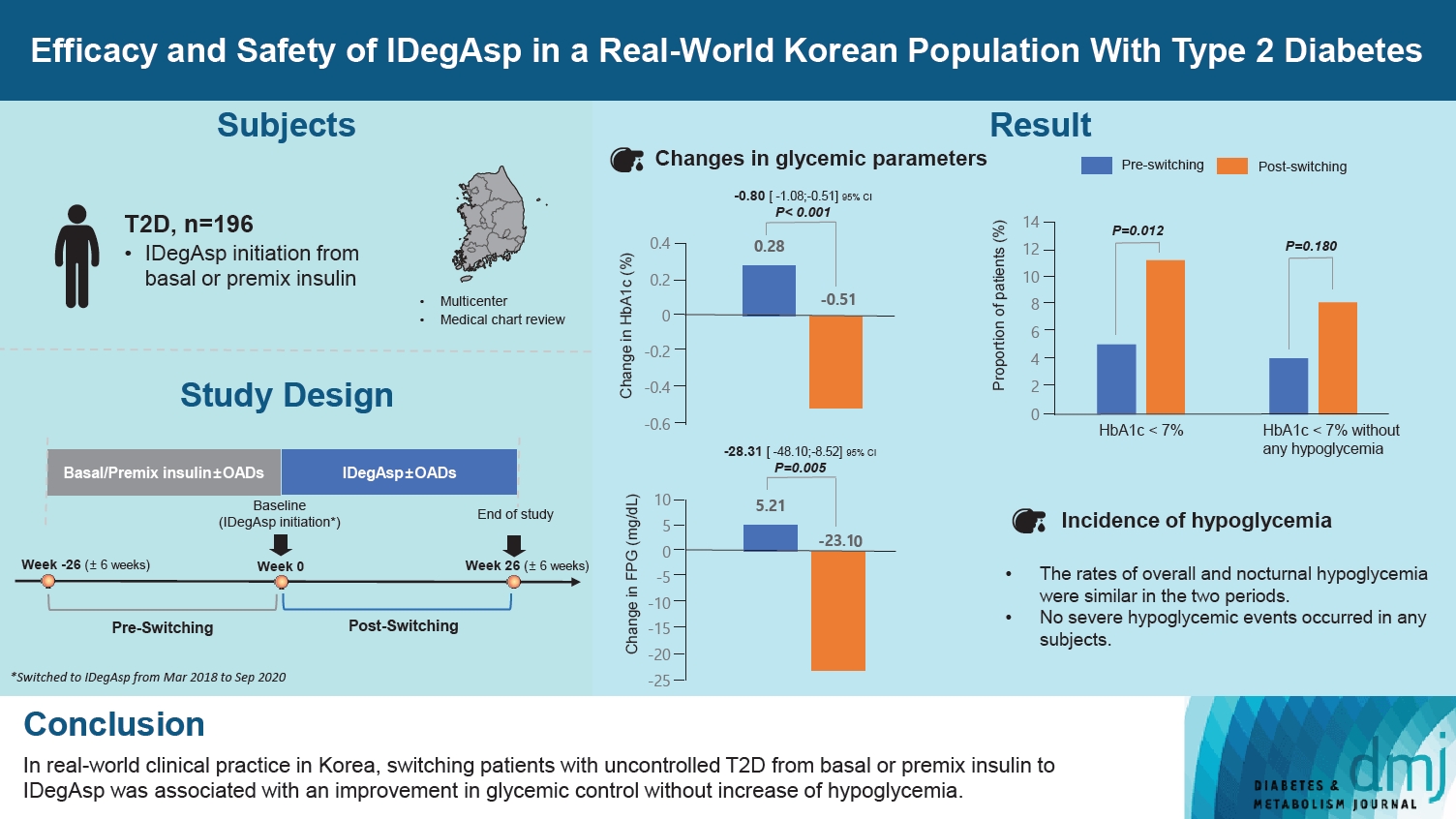
This study investigated the real-world efficacy and safety of insulin degludec/insulin aspart (IDegAsp) in Korean adults with type 2 diabetes mellitus (T2DM), whose insulin treatment was switched to IDegAsp.
Methods
This was a multicenter, retrospective, observational study comprising two 26-week treatment periods, before and after switching to IDegAsp, respectively. Korean adults with uncontrolled T2DM treated with basal or premix insulin (±oral antidiabetic drugs) were enrolled. The primary objective was to compare the degree of glycosylated hemoglobin (HbA1c) change in each 26-week observation period. The analyses included changes in HbA1c, fasting plasma glucose (FPG), body weight, proportion of participants achieving HbA1c <7.0%, hypoglycemic events, and total daily insulin dose (ClinicalTrials.gov, number NCT04656106).
Results
In total, 196 adults (mean age, 65.95 years; mean T2DM duration, 18.99 years) were analyzed. The change in both HbA1c and FPG were significantly different between the pre-switching and the post-switching period (0.28% vs. –0.51%, P<0.001; 5.21 mg/dL vs. –23.10 mg/dL, P=0.005), respectively. After switching, the rate of achieving HbA1c <7.0% was significantly improved (5.10% at baseline vs. 11.22% with IDegAsp, P=0.012). No significant differences (before vs. after switching) were observed in body weight change, and total daily insulin dose. The rates of overall and severe hypoglycemia were similar in the two periods.
Conclusion
In real-world clinical practice in Korea, the change of insulin regimen to IDegAsp was associated with an improvement in glycemic control without increase of hypoglycemia, supporting the use of IDegAsp for patients with T2DM uncontrolled with basal or premix insulin.
- Metabolic Risk/Epidemiology
- Higher Muscle Mass Protects Women with Gestational Diabetes Mellitus from Progression to Type 2 Diabetes Mellitus
- Yujin Shin, Joon Ho Moon, Tae Jung Oh, Chang Ho Ahn, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
- Diabetes Metab J. 2022;46(6):890-900. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0334
- 4,752 View
- 228 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We evaluated whether postpartum muscle mass affects the risk of type 2 diabetes mellitus (T2DM) in Korean women with gestational diabetes mellitus (GDM).
Methods
A total of 305 women with GDM (mean age, 34.9 years) was prospectively evaluated for incident prediabetes and T2DM from 2 months after delivery and annually thereafter. Appendicular skeletal muscle mass (ASM) was assessed with bioelectrical impedance analysis at the initial postpartum visit, and ASM, either divided by body mass index (BMI) or squared height, and the absolute ASM were used as muscle mass indices. The risk of incident prediabetes and T2DM was assessed according to tertiles of these indices using a logistic regression model.
Results
After a mean follow-up duration of 3.3 years, the highest ASM/BMI tertile group had a 61% lower risk of incident prediabetes and T2DM compared to the lowest tertile group, and this remained significant after we adjusted for covariates (adjusted odds ratio, 0.37; 95% confidence interval [CI], 0.15 to 0.92; P=0.032). Equivalent findings were observed in normal weight women (BMI <23 kg/m2), but this association was not significant for overweight women (BMI ≥23 kg/m2). Absolute ASM or ASM/height2 was not associated with the risk of postpartum T2DM.
Conclusion
A higher muscle mass, as defined by the ASM/BMI index, was associated with a lower risk of postpartum prediabetes and T2DM in Korean women with GDM. -
Citations
Citations to this article as recorded by- More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
Melanie S. Haines, Aaron Leong, Bianca C. Porneala, Victor W. Zhong, Cora E. Lewis, Pamela J. Schreiner, Karen K. Miller, James B. Meigs, Mercedes R. Carnethon
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(1): 105. CrossRef - The Association of the Triglyceride and Muscle to Fat Ratio During Early Pregnancy with the Development of Gestational Diabetes Mellitus
Fang Wang, Yuan-Yuan Bao, Kang Yu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3187. CrossRef - Correlation of body composition in early pregnancy on gestational diabetes mellitus under different body weights before pregnancy
Li Xintong, Xu Dongmei, Zhang Li, Cao Ruimin, Hao Yide, Cui Lingling, Chen Tingting, Guo Yingying, Li Jiaxin
Frontiers in Endocrinology.2022;[Epub] CrossRef
- More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
- Metabolic Risk/Epidemiology
- Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
- Joon Ho Moon, Hak Chul Jang
- Diabetes Metab J. 2022;46(1):3-14. Published online January 27, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0335
- 14,591 View
- 888 Download
- 54 Web of Science
- 61 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 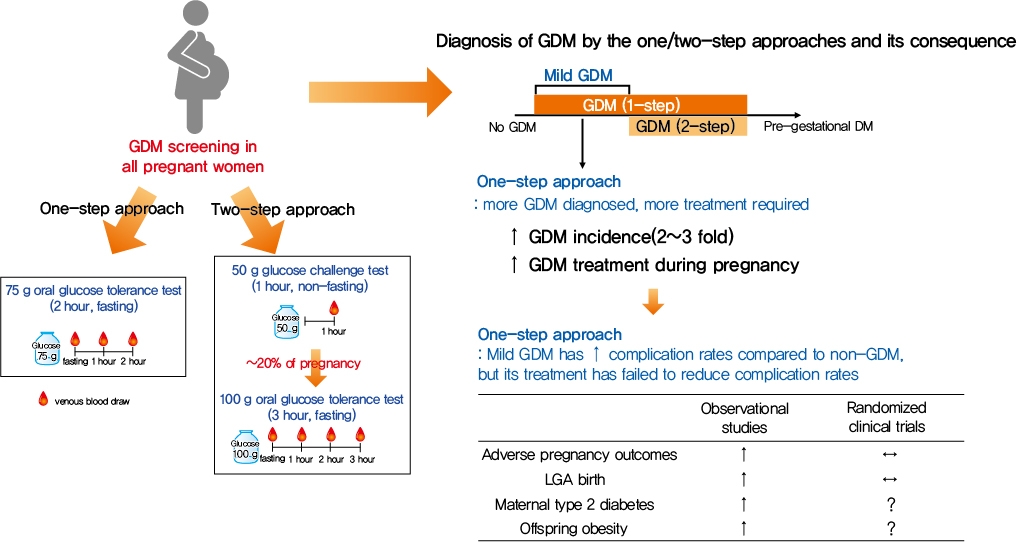
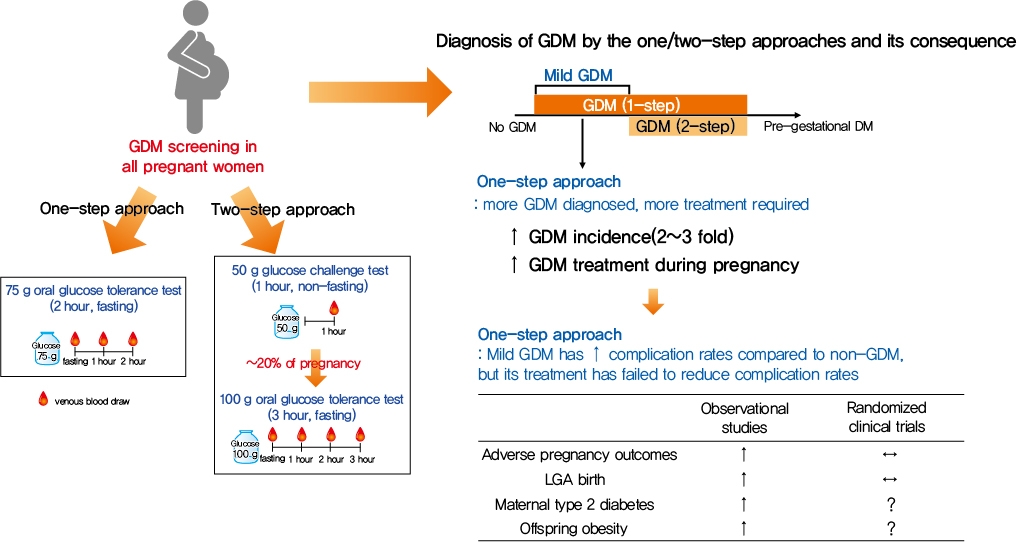
- Gestational diabetes mellitus (GDM) is the most common complication during pregnancy and is defined as any degree of glucose intolerance with onset or first recognition during pregnancy. GDM is associated with adverse pregnancy outcomes and long-term offspring and maternal complications. For GDM screening and diagnosis, a two-step approach (1-hour 50 g glucose challenge test followed by 3-hour 100 g oral glucose tolerance test) has been widely used. After the Hyperglycemia and Adverse Pregnancy Outcome study implemented a 75 g oral glucose tolerance test in all pregnant women, a one-step approach was recommended as an option for the diagnosis of GDM after 2010. The one-step approach has more than doubled the incidence of GDM, but its clinical benefit in reducing adverse pregnancy outcomes remains controversial. Long-term complications of mothers with GDM include type 2 diabetes mellitus and cardiovascular disease, and complications of their offspring include childhood obesity and glucose intolerance. The diagnostic criteria of GDM should properly classify women at risk for adverse pregnancy outcomes and long-term complications. The present review summarizes the strengths and weaknesses of the one-step and two-step approaches for the diagnosis of GDM based on recent randomized controlled trials and observational studies. We also describe the long-term maternal and offspring complications of GDM.
-
Citations
Citations to this article as recorded by- Prophylactic administration of metformin reduces gestational diabetes mellitus incidence in the high-risk populations: a meta-analysis
Hui Yu, Jinling Sun, Honglei Hu
Irish Journal of Medical Science (1971 -).2024; 193(1): 199. CrossRef - Association of dietary inflammatory index with risk of gestational diabetes mellitus and preeclampsia: a systematic review and meta-analysis
Li Hong, Liyuan Zhu, Jinru Zhang, Yueqi Fu, Xiaoyan Qi, Mei Zhao
British Journal of Nutrition.2024; 131(1): 54. CrossRef - Ferritin and iron supplements in gestational diabetes mellitus: less or more?
Tianlian Li, Jingfan Zhang, Ping Li
European Journal of Nutrition.2024; 63(1): 67. CrossRef - Comparing the screening methods for gestational diabetes mellitus before and during the COVID‐19 pandemic: A systematic review
Xingge Sun, Clare McKeaveney, Helen Noble, Hannah O’Hara, Oliver Perra
Journal of Diabetes Investigation.2024; 15(4): 500. CrossRef - Protective Effects of Paeoniflorin Against Inflammation and Oxidative Stress in Rats with Gestational Diabetes Mellitus via Inhibiting the RhoA/ROCK Signaling Pathway
Cheng kun Yuan, Yan Gao, Jinglu Yu, Limin Peng
Revista Brasileira de Farmacognosia.2024;[Epub] CrossRef - METTL14‐mediated lncRNA XIST silencing alleviates GDM progression by facilitating trophoblast cell proliferation and migration via the miR‐497‐5p/FOXO1 axis
Yanchuan Li, Yanfeng Liu, Xiao Yao, Haili Wang, Ziyun Shi, Meiqing He
Journal of Biochemical and Molecular Toxicology.2024;[Epub] CrossRef - Evaluation of insulin secretion and insulin sensitivity in pregnant women: Application value of simple indices
Shuying Ren, Dan Wu, Ping Li
Clinica Chimica Acta.2024; 554: 117753. CrossRef - ATP5me alleviates high glucose-induced myocardial cell injury
Qingsha Hou, Fang Yan, Xiuling Li, Huanling Liu, Xiang Yang, Xudong Dong
International Immunopharmacology.2024; 129: 111626. CrossRef - Aberrant NK cell profile in gestational diabetes mellitus with fetal growth restriction
Yujing Xiong, Yazhen Wang, Mengqi Wu, Shuqiang Chen, Hui Lei, Hui Mu, Haikun Yu, Yongli Hou, Kang Tang, Xutao Chen, Jie Dong, Xiaohong Wang, Lihua Chen
Frontiers in Immunology.2024;[Epub] CrossRef - Maternal Diabetes and Risk of Hypospadias: A Systemic Review and Meta-Analysis
Zhiyuan Liu, Chengjun Yu, Shuhan Yang, Jin Luo, Jie Zhang, Xiao Wang, Chun Wei, Qinlin Shi, Yi Hua, Xing Liu, Guanghui Wei
Urologia Internationalis.2024; 108(2): 108. CrossRef - Maternal birth weight as an indicator of early and late gestational diabetes mellitus: The Japan Environment and Children's Study
Kazuma Tagami, Noriyuki Iwama, Hirotaka Hamada, Hasumi Tomita, Rie Kudo, Natsumi Kumagai, Hongxin Wang, Seiya Izumi, Zen Watanabe, Mami Ishikuro, Taku Obara, Nozomi Tatsuta, Hirohito Metoki, Chiharu Ota, Takashi Sugiyama, Shinichi Kuriyama, Takahiro Arima
Journal of Diabetes Investigation.2024;[Epub] CrossRef - Perinatal characteristics and pregnancy outcomes of advanced maternal age women with gestational diabetes mellitus: A retrospective cohort study
Chen Jiang, Haiyan Wen, Tingting Hu, Yanfei Liu, Xiaoqing Dai, Yiming Chen
Health Science Reports.2024;[Epub] CrossRef - Phenotypic characterisation of regulatory T cells in patients with gestational diabetes mellitus
Ya-nan Zhang, Qin Wu, Yi-hui Deng
Scientific Reports.2024;[Epub] CrossRef - Healthy behaviors and gestational diabetes mellitus in an Iranian setting: A cross-sectional study
Maryam Zare, Afrouz Mardi, Paria Yeghanenia, Daniel Hackett
Medicine.2024; 103(9): e36431. CrossRef - Post‐load glucose is a stronger predictor of adverse pregnancy outcomes than first‐trimester HbA1c in women without gestational diabetes
Shahin Keshtkar Rajabi, Elham Toghraee, Golnoosh Nejatipour
Journal of Diabetes Investigation.2024;[Epub] CrossRef - Triglyceride-glucose index in early pregnancy predicts the risk of gestational diabetes: a prospective cohort study
Yufeng Guo, Junwen Lu, Mailiman Bahani, Guifeng Ding, Lei Wang, Yuxia Zhang, Huanmei Zhang, Chengyao Liu, Lijun Zhou, Xiaolan Liu, Fangshen Li, Xiaoli Wang, Hong Ding
Lipids in Health and Disease.2024;[Epub] CrossRef - A study on behavior, diet patterns and physical activity among selected GDM and non-GDM women in south India
S Sindhu, S Uma Mageshwari
Journal of Diabetology.2024; 15(1): 86. CrossRef - The Implication of Diabetes-Specialized Nurses in Aiming for the Better Treatment and Management of Patients with Diabetes Mellitus: A Brief Narrative Review
Yefang Zhu, Hongmei Zhang, Ying Xi, Hongli Zhu, Yan Lu, Xue Luo, Zhangui Tang, Hong Lei
Diabetes Therapy.2024;[Epub] CrossRef - Triglyceride-glucose index: A promising biomarker for predicting risks of adverse pregnancy outcomes in Hangzhou, China
Jinghua Zhang, Binbin Yin, Ya Xi, Yongying Bai
Preventive Medicine Reports.2024; 41: 102683. CrossRef - Associations of education attainment with gestational diabetes mellitus and the mediating effects of obesity: A Mendelian randomization study
Xiaoyan Wang, Ying Lan, Na Li, Jinfeng Gao, Dejiao Meng, Shuchuan Miao
Heliyon.2024; 10(7): e29000. CrossRef - Quality assessment of videos on social media platforms related to gestational diabetes mellitus in China: A cross-section study
Qin-Yu Cai, Jing Tang, Si-Zhe Meng, Yi Sun, Xia Lan, Tai-Hang Liu
Heliyon.2024; 10(7): e29020. CrossRef - One abnormal value in oral glucose tolerance test during pregnancy and type 2 diabetes risk: Insights from a 5-Year Follow-Up study
Rawia Hussein-Aro, Esther Maor-Sagie, Yoel Toledano, Mordechai Hallak, Rinat Gabbay-Benziv
Diabetes Research and Clinical Practice.2024; 211: 111659. CrossRef - Assessment of the Level of Knowledge About Risk Factors, Prevention, and Treatment of Gestational Diabetes Mellitus in a Community Sample From Saudi Arabia
Suzan A Morsy, Ayat M Tawfik, Samar Y Badayyan, Lameer K Shaikh, Shaden AzizKhan, AlKhansaa A Zakari
Cureus.2024;[Epub] CrossRef - Genetic Susceptibility, Mendelian Randomization, and Nomogram Model Construction of Gestational Diabetes Mellitus
Qiulian Liang, Ming Li, Gongchen Huang, Ruiqi Li, Linyuan Qin, Ping Zhong, Xuekun Xing, Xiangyuan Yu
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Study on the regulation of trophoblast activity by abnormally expressed hsa_circ_0024838/miR-543/HIF1A in patients with gestational diabetes mellitus
Qian Liu, Faminzi Li, Juan Gui, Lianzhi Wu
Placenta.2024;[Epub] CrossRef - U-shaped Association Between Folic Acid Supplementation and the Risk of Gestational Diabetes Mellitus in Chinese Women
Jiuming Zou, Qiang Fu, Xiaoliu Huang, Zhao Yao, Weiye Wang
Canadian Journal of Diabetes.2023; 47(1): 78. CrossRef - Vitamin D Supplementation for the Outcomes of Patients with Gestational Diabetes Mellitus and Neonates: A Meta-Analysis and Systematic Review
Chunfeng Wu, Yang Song, Xueying Wang, Pier P. Sainaghi
International Journal of Clinical Practice.2023; 2023: 1. CrossRef - Lipolysis and gestational diabetes mellitus onset: a case-cohort genome-wide association study in Chinese
Miao Zhang, Qing Li, Kai-Lin Wang, Yao Dong, Yu-Tong Mu, Yan-Min Cao, Jin Liu, Zi-Heng Li, Hui-Lu Cui, Hai-Yan Liu, An-Qun Hu, Ying-Jie Zheng
Journal of Translational Medicine.2023;[Epub] CrossRef - Interactive effect of prepregnancy overweight/obesity and GDM history on prevalence of GDM in biparous women
Xia Xu, Feipeng Huang, Yanni Guo, Lianghui Zheng, Jianying Yan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Microbiome Changes in Pregnancy Disorders
Luca Giannella, Camilla Grelloni, Dayana Quintili, Alessia Fiorelli, Ramona Montironi, Sonila Alia, Giovanni Delli Carpini, Jacopo Di Giuseppe, Arianna Vignini, Andrea Ciavattini
Antioxidants.2023; 12(2): 463. CrossRef - Effects of early standardized management on the growth trajectory of offspring with gestational diabetes mellitus at 0–5 years old: a preliminary longitudinal study
Bingbing Guo, Jingjing Pei, Yin Xu, Yajie Wang, Xinye Jiang
Scientific Reports.2023;[Epub] CrossRef - Prediction model for gestational diabetes mellitus using the XG Boost machine learning algorithm
Xiaoqi Hu, Xiaolin Hu, Ya Yu, Jia Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Prevalence and outcomes of gestational diabetes mellitus in Indian women: Insights from a large real-world study over ten years at tertiary care research institute
Sanjay Gupte, Gayatri Venkataraman, Aarti S. Shah, Shalaka Jamenis, Chandrakant Rao, Shweta M. Jangam, Kaveri M. Adki, Onkar C. Swami
International Journal of Diabetes in Developing Countries.2023; 43(4): 511. CrossRef - Gestational diabetes mellitus: state of art
S. A. Pletneva, E. V. Enkova, O. V. Khoperskaya, S. V. Shamarin, V. V. Enkova
Meditsinskiy sovet = Medical Council.2023; (5): 136. CrossRef - Effect of folic acid supplementation in the association between short sleep duration and gestational diabetes mellitus
Zhen Yang, Sisi Hu, Wei Tong, Zhihao Xu, Xiaoliu Huang, Weiye Wang
Sleep and Breathing.2023; 27(6): 2509. CrossRef - Birth weight and large for gestational age trends in offspring of pregnant women with gestational diabetes mellitus in southern China, 2012-2021
Li-Rong He, Li Yu, Yong Guo
Frontiers in Endocrinology.2023;[Epub] CrossRef - Root causes of long-term complications of gestational diabetes mellitus: Metabolic disturbances of the host and gut microbiota
Mingjin Tao, Gaochen Lu, Sheng Zhang, Pan Li
Clinica Chimica Acta.2023; 548: 117490. CrossRef - Analysis on Related Risk Factors for Gestational Diabetes Mellitus (GDM) in Subsequent Pregnancies in Multiparous Women with No History of GDM
文静 张
Advances in Clinical Medicine.2023; 13(07): 11628. CrossRef - Fetoplacental endothelial dysfunction in gestational diabetes mellitus and maternal obesity: A potential threat for programming cardiovascular disease
Mariana S. Diniz, Ursula Hiden, Inês Falcão-Pires, Paulo J. Oliveira, Luis Sobrevia, Susana P. Pereira
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2023; 1869(8): 166834. CrossRef - Diagnosis and management of gestational diabetes mellitus
Tae Jung Oh
Journal of the Korean Medical Association.2023; 66(7): 414. CrossRef - Hypoglycemia in Children: Major Endocrine-Metabolic Causes and Novel Therapeutic Perspectives
Alessia Quarta, Daniela Iannucci, Miriana Guarino, Annalisa Blasetti, Francesco Chiarelli
Nutrients.2023; 15(16): 3544. CrossRef - Relation between weight gain during pregnancy and postpartum reclassification in gestational diabetes
Sofia Coelho, Marta Canha, Ana Rita Leite, João Sérgio Neves, Ana Isabel Oliveira, Davide Carvalho, Maria do Céu Ameida
Endocrine.2023; 82(2): 296. CrossRef - Nurturing through Nutrition: Exploring the Role of Antioxidants in Maternal Diet during Pregnancy to Mitigate Developmental Programming of Chronic Diseases
Mariana S. Diniz, Carina C. Magalhães, Carolina Tocantins, Luís F. Grilo, José Teixeira, Susana P. Pereira
Nutrients.2023; 15(21): 4623. CrossRef - Blood manganese level and gestational diabetes mellitus: a systematic review and meta-analysis
Yingmei Sun, Yu Zhang
Journal of Obstetrics and Gynaecology.2023;[Epub] CrossRef - Multiparity increases the risk of diabetes by impairing the proliferative capacity of pancreatic β cells
Joon Ho Moon, Joonyub Lee, Kyun Hoo Kim, Hyun Jung Kim, Hyeongseok Kim, Hye-Na Cha, Jungsun Park, Hyeonkyu Lee, So-young Park, Hak Chul Jang, Hail Kim
Experimental & Molecular Medicine.2023; 55(10): 2269. CrossRef - Physiological Mechanisms Inherent to Diabetes Involved in the Development of Dementia: Alzheimer’s Disease
Himan Mohamed-Mohamed, Victoria García-Morales, Encarnación María Sánchez Lara, Anabel González-Acedo, Teresa Pardo-Moreno, María Isabel Tovar-Gálvez, Lucía Melguizo-Rodríguez, Juan José Ramos-Rodríguez
Neurology International.2023; 15(4): 1253. CrossRef - Synergistic effect between pre-pregnancy smoking and assisted reproductive technology on gestational diabetes mellitus in twin pregnancies
Lingyu Zhang, Yan Huang, Mingjin Zhang, Yanqi Jin
Acta Diabetologica.2023; 61(2): 205. CrossRef - A Comprehensive Review of Gestational Diabetes Mellitus: Impacts on Maternal Health, Fetal Development, Childhood Outcomes, and Long-Term Treatment Strategies
Vaishnavi S Nakshine, Sangita D Jogdand
Cureus.2023;[Epub] CrossRef - The role of dietary fiber on preventing gestational diabetes mellitus in an at-risk group of high triglyceride-glucose index women: a randomized controlled trial
Yannan Cao, Jing Sheng, Dongyao Zhang, Li Chen, Ying Jiang, Decui Cheng, Yao Su, Yuexin Yu, Haoyi Jia, Pengyuan He, Li Wang, Xianming Xu
Endocrine.2023; 82(3): 542. CrossRef - Correlation between PAPP-A serum levels in the first trimester of pregnancy with the occurrence of gestational diabetes, a multicenter cohort study
Sedigheh Borna, Masoumeh Ashrafzadeh, Marjan Ghaemi, Nasim Eshraghi, Nafiseh Hivechi, Sedigheh Hantoushzadeh
BMC Pregnancy and Childbirth.2023;[Epub] CrossRef - Impact of COVID-19 lockdown on glycemic levels during pregnancy: A retrospective analysis
Erika Di Zazzo, Sergio Davinelli, Serena Panichella, Giovanni Scapagnini, Mariano Intrieri, Silvio Garofalo
Open Medicine.2023;[Epub] CrossRef - Advancements in Nutritional Strategies for Gestational Diabetes Management: A Systematic Review of Recent Evidence
Juan Carlos Sánchez-García, Ines Saraceno López-Palop, Beatriz Piqueras-Sola, Jonathan Cortés-Martín, Elena Mellado-García, Inmaculada Muñóz Sánchez, Raquel Rodríguez-Blanque
Journal of Clinical Medicine.2023; 13(1): 37. CrossRef - Comparative efficacy and safety of glyburide, metformin, and insulin in treatment of gestational diabetes mellitus
Jing Lin, Rong-zu Tu, Xun-yu Hong
Medicine.2022;[Epub] CrossRef - Stacking Ensemble Method for Gestational Diabetes Mellitus Prediction in Chinese Pregnant Women: A Prospective Cohort Study
Ruiyi Liu, Yongle Zhan, Xuan Liu, Yifang Zhang, Luting Gui, Yimin Qu, Hairong Nan, Yu Jiang, Mehdi Gheisari
Journal of Healthcare Engineering.2022; 2022: 1. CrossRef - Secular increase in the prevalence of gestational diabetes and its associated adverse pregnancy outcomes from 2014 to 2021 in Hebei province, China
Mei-Ling Tian, Li-Yan Du, Guo-Juan Ma, Ting Zhang, Xu-Yuan Ma, Ying-Kui Zhang, Zeng-Jun Tang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Aquaporin-8 overexpression is involved in vascular structure and function changes in placentas of gestational diabetes mellitus patients
Yanxing Shan, Jiawen Cui, Xinyi Kang, Weichun Tang, Yiling Lu, Ying Gao, Liping Chen
Open Life Sciences.2022; 17(1): 1473. CrossRef - Vitamin D status and levels of pro-inflammatory cytokines in newborns born to mothers with endocrine diseases
N. E. Verisokina, L. Ya. Klimov, I. N. Zakharova, A. L. Zaplatnikov, V. V. Zubkov, A. A. Momotova, V. A. Kuryaninova, R. A. Atanesyan, T. V. Zhelezniakova, M. A. Petrosyan, D. V. Bobryshev, D. A. Volkov, Z. A. Magomadova
Meditsinskiy sovet = Medical Council.2022; (19): 9. CrossRef - IL-6 and IL-8: An Overview of Their Roles in Healthy and Pathological Pregnancies
Aleksandra Vilotić, Mirjana Nacka-Aleksić, Andrea Pirković, Žanka Bojić-Trbojević, Dragana Dekanski, Milica Jovanović Krivokuća
International Journal of Molecular Sciences.2022; 23(23): 14574. CrossRef - Higher Muscle Mass Protects Women with Gestational Diabetes Mellitus from Progression to Type 2 Diabetes Mellitus
Yujin Shin, Joon Ho Moon, Tae Jung Oh, Chang Ho Ahn, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Diabetes & Metabolism Journal.2022; 46(6): 890. CrossRef - Identification of human placenta-derived circular RNAs and autophagy related circRNA-miRNA-mRNA regulatory network in gestational diabetes mellitus
Yindi Bao, Jun Zhang, Yi Liu, Lianzhi Wu, Jing Yang
Frontiers in Genetics.2022;[Epub] CrossRef - The Role of Dietary Polyphenols in Pregnancy and Pregnancy-Related Disorders
Mirjana Nacka-Aleksić, Andrea Pirković, Aleksandra Vilotić, Žanka Bojić-Trbojević, Milica Jovanović Krivokuća, Francesca Giampieri, Maurizio Battino, Dragana Dekanski
Nutrients.2022; 14(24): 5246. CrossRef
- Prophylactic administration of metformin reduces gestational diabetes mellitus incidence in the high-risk populations: a meta-analysis
- Technology/Device
- Glucose Profiles Assessed by Intermittently Scanned Continuous Glucose Monitoring System during the Perioperative Period of Metabolic Surgery
- Kyuho Kim, Sung Hee Choi, Hak Chul Jang, Young Suk Park, Tae Jung Oh
- Diabetes Metab J. 2022;46(5):713-721. Published online January 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0164
- 4,790 View
- 317 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
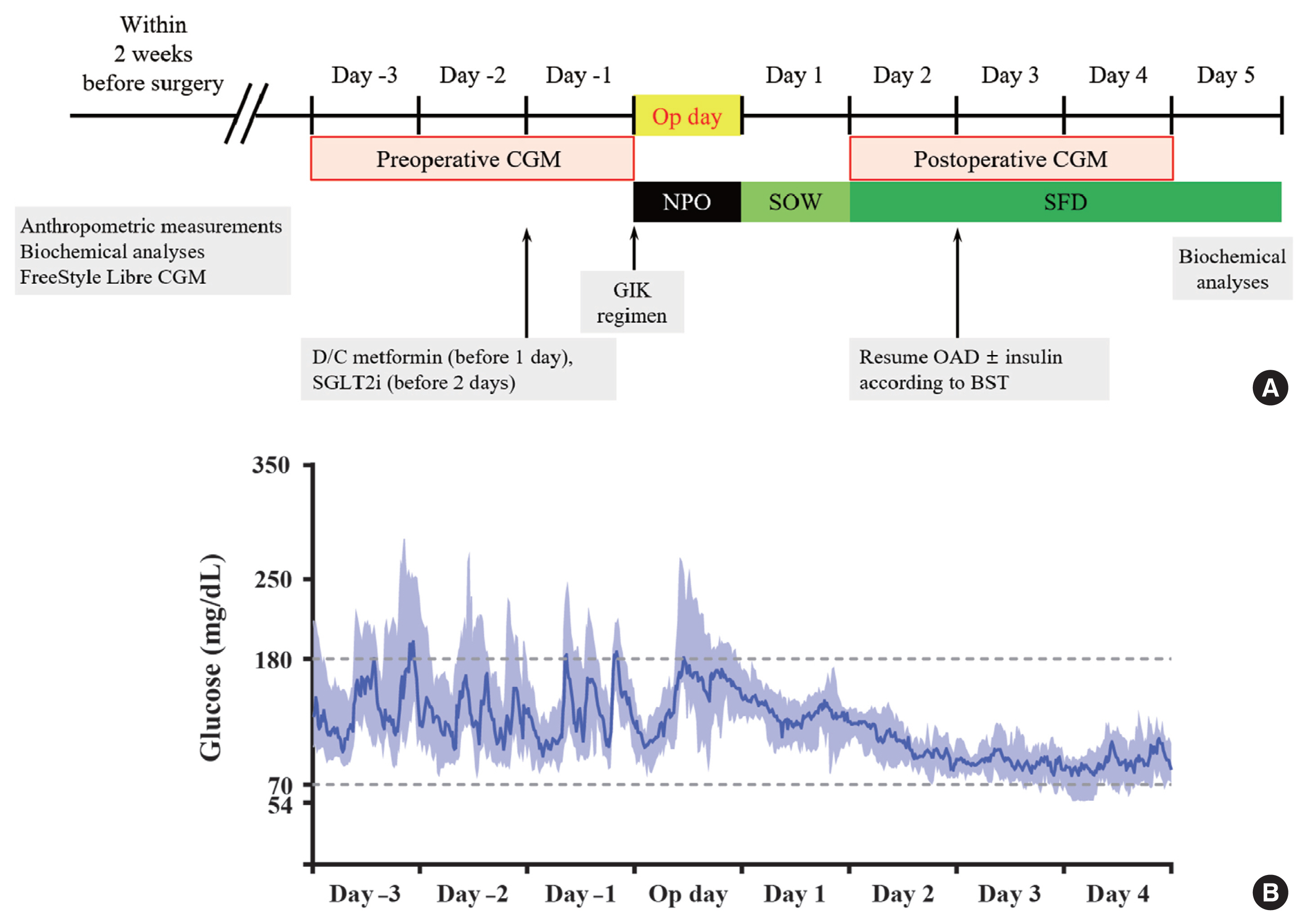
Continuous glucose monitoring (CGM) has been widely used in the management of diabetes. However, the usefulness and detailed data during perioperative status were not well studied. In this study, we described the immediate changes of glucose profiles after metabolic surgery using intermittently scanned CGM (isCGM) in individuals with type 2 diabetes mellitus (T2DM).
Methods
This was a prospective, single-center, single-arm study including 20 participants with T2DM. The isCGM (FreeStyle Libre CGM) implantation was performed within 2 weeks before surgery. We compared CGM metrics of 3 days before surgery and 3 days after surgery, and performed the correlation analyses with clinical variables.
Results
The mean glucose significantly decreased after surgery (147.0±40.4 to 95.5±17.1 mg/dL, P<0.001). Time in range (TIR; 70 to 180 mg/dL) did not significantly change after surgery in total. However, it was significantly increased in a subgroup of individuals with glycosylated hemoglobin (HbA1c) ≥8.0%. Time above range (>250 or 180 mg/dL) was significantly decreased in total. In contrast, time below range (<70 or 54 mg/dL) was significantly increased in total and especially in a subgroup of individuals with HbA1c <8.0% after surgery. The coefficient of variation significantly decreased after surgery. Higher baseline HbA1c was correlated with greater improvement in TIR (rho=0.607, P=0.005).
Conclusion
The isCGM identified improvement of mean glucose and glycemic variability, and increase of hypoglycemia after metabolic surgery, but TIR was not significantly changed after surgery. We detected an increase of TIR only in individuals with HbA1c ≥8.0%. -
Citations
Citations to this article as recorded by- Comparative Effect of Glucose-Lowering Drugs for Type 2 Diabetes Mellitus on Stroke Prevention: A Systematic Review and Network Meta-Analysis
Ji Soo Kim, Gyeongsil Lee, Kyung-Il Park, Seung-Won Oh
Diabetes & Metabolism Journal.2024; 48(2): 312. CrossRef - Use of Continuous Glucose Monitoring in Patients Following Bariatric Surgery: A Scoping Review
Yang Yu, Susan W. Groth
Obesity Surgery.2023; 33(8): 2573. CrossRef - Asymptomatic Hypoglycemia after Metabolic Surgery: New Insights from Perioperative Continuous Glucose Monitoring
Sang-Man Jin
Diabetes & Metabolism Journal.2022; 46(5): 675. CrossRef
- Comparative Effect of Glucose-Lowering Drugs for Type 2 Diabetes Mellitus on Stroke Prevention: A Systematic Review and Network Meta-Analysis
- Complications
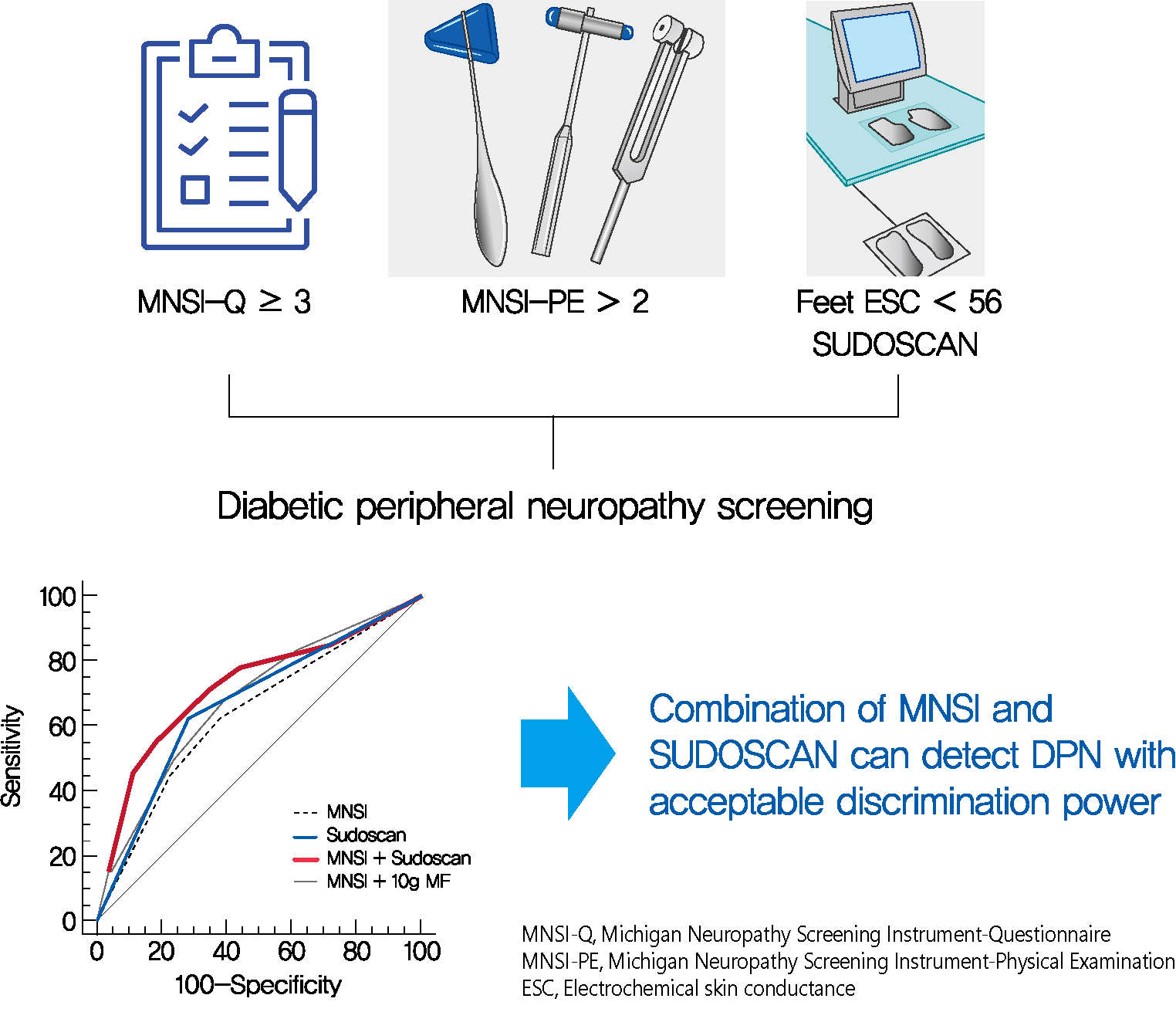
- SUDOSCAN in Combination with the Michigan Neuropathy Screening Instrument Is an Effective Tool for Screening Diabetic Peripheral Neuropathy
- Tae Jung Oh, Yoojung Song, Hak Chul Jang, Sung Hee Choi
- Diabetes Metab J. 2022;46(2):319-326. Published online September 16, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0014
- 5,822 View
- 314 Download
- 11 Web of Science
- 12 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 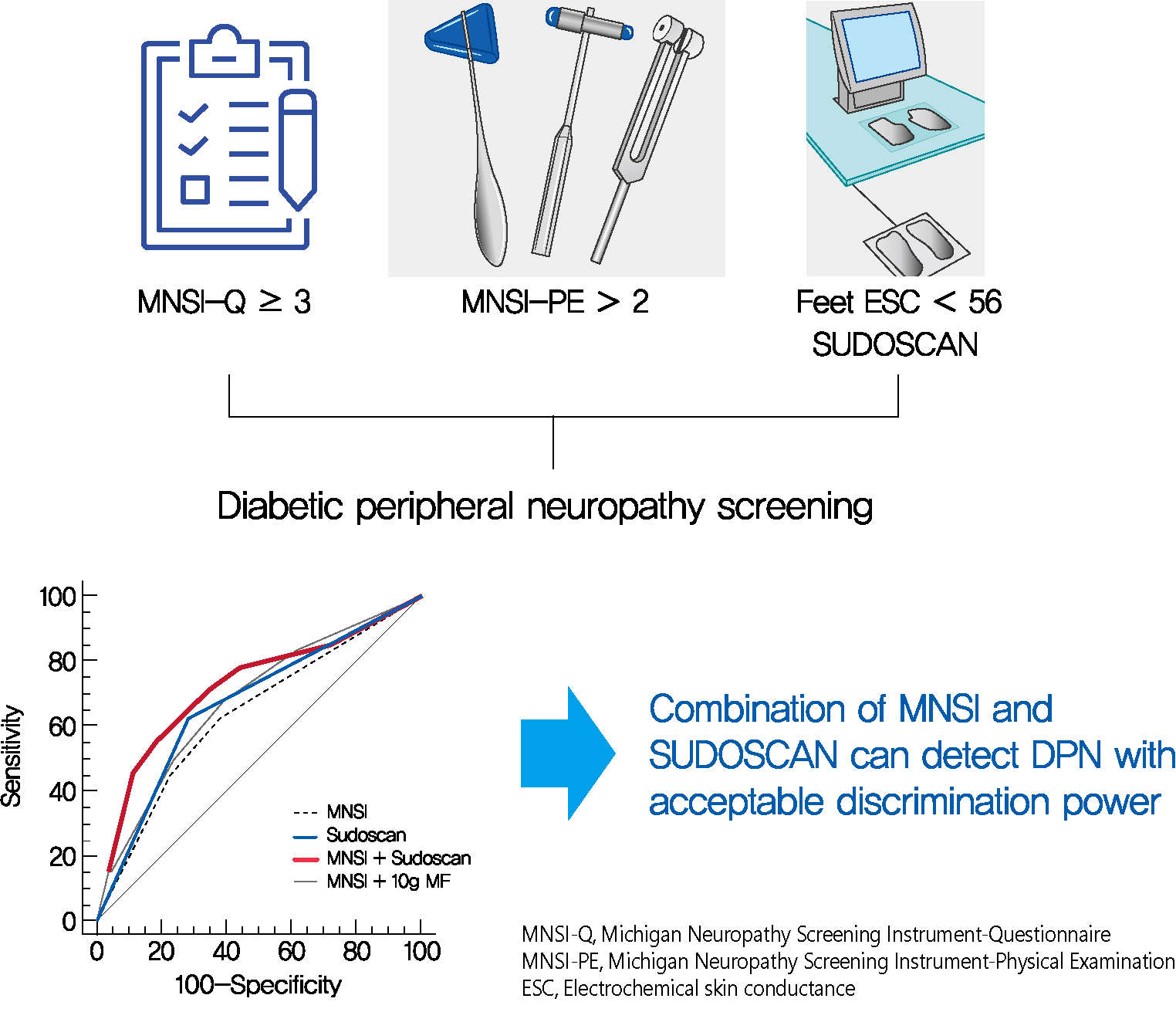
- Background
Screening for diabetic peripheral neuropathy (DPN) is important to prevent severe foot complication, but the detection rate of DPN is unsatisfactory. We investigated whether SUDOSCAN combined with Michigan Neuropathy Screening Instrument (MNSI) could be an effective tool for screening for DPN in people with type 2 diabetes mellitus (T2DM) in clinical practice.
Methods
We analysed the data for 144 people with T2DM without other cause of neuropathy. The presence of DPN was confirmed according to the Toronto Consensus criteria. Electrochemical skin conductance (ESC) of the feet was assessed using SUDOSCAN. We compared the discrimination power of following methods, MNSI only vs. SUDOSCAN only vs. MNSI plus SUDOSCAN vs. MNSI plus 10-g monofilament test.
Results
Confirmed DPN was detected in 27.8% of the participants. The optimal cut-off value of feet ESC to distinguish DPN was 56 μS. We made the DPN screening scores using the corresponding odds ratios for MNSI-Questionnaire, MNSI-Physical Examination, SUDOSCAN, and 10-g monofilament test. For distinguishing the presence of DPN, the MNSI plus SUDOSCAN model showed higher areas under the receiver operating characteristic curve (AUC) than MNSI only model (0.717 vs. 0.638, P=0.011), and SUDOSCAN only model or MNSI plus 10-g monofilament test showed comparable AUC with MNSI only model.
Conclusion
The screening model for DPN that includes both MNSI and SUDOSCAN can detect DPN with acceptable discrimination power and it may be useful in Korean patients with T2DM. -
Citations
Citations to this article as recorded by- Association of sudomotor dysfunction with risk of diabetic retinopathy in patients with type 2 diabetes
Ming Wang, Niuniu Chen, Yaxin Wang, Jiaying Ni, Jingyi Lu, Weijing Zhao, Yating Cui, Ronghui Du, Wei Zhu, Jian Zhou
Endocrine.2024;[Epub] CrossRef - Vitamin D deficiency increases the risk of diabetic peripheral neuropathy in elderly type 2 diabetes mellitus patients by predominantly increasing large-fiber lesions
Sijia Fei, Jingwen Fan, Jiaming Cao, Huan Chen, Xiaoxia Wang, Qi Pan
Diabetes Research and Clinical Practice.2024; 209: 111585. CrossRef - Peripheral Neuropathy in Diabetes Mellitus: Pathogenetic Mechanisms and Diagnostic Options
Raffaele Galiero, Alfredo Caturano, Erica Vetrano, Domenico Beccia, Chiara Brin, Maria Alfano, Jessica Di Salvo, Raffaella Epifani, Alessia Piacevole, Giuseppina Tagliaferri, Maria Rocco, Ilaria Iadicicco, Giovanni Docimo, Luca Rinaldi, Celestino Sardu, T
International Journal of Molecular Sciences.2023; 24(4): 3554. CrossRef - Screening for diabetic peripheral neuropathy in resource-limited settings
Ken Munene Nkonge, Dennis Karani Nkonge, Teresa Njeri Nkonge
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - The value of electrochemical skin conductance measurement by Sudoscan® for assessing autonomic dysfunction in peripheral neuropathies beyond diabetes
Jean-Pascal Lefaucheur
Neurophysiologie Clinique.2023; 53(2): 102859. CrossRef - Electrochemical skin conductances values and clinical factors affecting sudomotor dysfunction in patients with prediabetes, type 1 diabetes, and type 2 diabetes: A single center experience
Bedia Fulya Calikoglu, Selda Celik, Cemile Idiz, Elif Bagdemir, Halim Issever, Jean-Henri Calvet, Ilhan Satman
Primary Care Diabetes.2023; 17(5): 499. CrossRef - Autonomic Nerve Function Tests in Patients with Diabetes
Heung Yong Jin, Tae Sun Park
The Journal of Korean Diabetes.2023; 24(2): 71. CrossRef - Validation of the Body Scan®, a new device to detect small fiber neuropathy by assessment of the sudomotor function: agreement with the Sudoscan®
Jean-Pierre Riveline, Roberto Mallone, Clarisse Tiercelin, Fetta Yaker, Laure Alexandre-Heymann, Lysa Khelifaoui, Florence Travert, Claire Fertichon, Jean-Baptiste Julla, Tiphaine Vidal-Trecan, Louis Potier, Jean-Francois Gautier, Etienne Larger, Jean-Pas
Frontiers in Neurology.2023;[Epub] CrossRef - Electrochemical Skin Conductance by Sudoscan in Non-Dialysis Chronic Kidney Disease Patients
Liang-Te Chiu, Yu-Li Lin, Chih-Hsien Wang, Chii-Min Hwu, Hung-Hsiang Liou, Bang-Gee Hsu
Journal of Clinical Medicine.2023; 13(1): 187. CrossRef - The Presence of Clonal Hematopoiesis Is Negatively Associated with Diabetic Peripheral Neuropathy in Type 2 Diabetes
Tae Jung Oh, Han Song, Youngil Koh, Sung Hee Choi
Endocrinology and Metabolism.2022; 37(2): 243. CrossRef - Case report: Significant relief of linezolid-induced peripheral neuropathy in a pre-XDR-TB case after acupuncture treatment
Yuping Mo, Zhu Zhu, Jie Tan, Zhilin Liang, Jiahui Wu, Xingcheng Chen, Ming Hu, Peize Zhang, Guofang Deng, Liang Fu
Frontiers in Neurology.2022;[Epub] CrossRef - Detection of sudomotor alterations evaluated by Sudoscan in patients with recently diagnosed type 2 diabetes
Ana Cristina García-Ulloa, Paloma Almeda-Valdes, Teresa Enedina Cuatecontzi-Xochitiotzi, Jorge Alberto Ramírez-García, Michelle Díaz-Pineda, Fernanda Garnica-Carrillo, Alejandra González-Duarte, K M Venkat Narayan, Carlos Alberto Aguilar-Salinas, Sergio H
BMJ Open Diabetes Research & Care.2022; 10(6): e003005. CrossRef
- Association of sudomotor dysfunction with risk of diabetic retinopathy in patients with type 2 diabetes
- COVID-19
- Effects of Social Distancing on Diabetes Management in Older Adults during COVID-19 Pandemic
- Soo Myoung Shin, Tae Jung Oh, Sung Hee Choi, Hak Chul Jang
- Diabetes Metab J. 2021;45(5):765-772. Published online August 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0096

- 5,957 View
- 191 Download
- 9 Web of Science
- 9 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
On March 22, 2020, intense social distancing (SD) was implemented in Korea to prevent the spread of coronavirus disease 19 (COVID-19). This study examined the impact of SD on diabetes control in older adults with diabetes.
Methods
Adults aged 60 to 90 years with type 2 diabetes mellitus who were physically and mentally independent were recruited. Participants who had complete blood chemistry data from April to July 2019 (pre-SD era) and April to July 2020 (SD era) were enrolled. Data were obtained about physical activity, nutrition, sarcopenia, and psychological and mental health from questionnaires in April to July 2020. Calf circumference was measured.
Results
In total, 246 people (100 men, 146 women; mean age, 73.8±5.7 years) participated in this study. The levels of glycated hemoglobin (HbA1c, 7.4%±1.0% vs. 7.1%±0.8%, P<0.001), fasting glucose (142.2±16.7 mg/dL vs. 132.0±27.7 mg/dL, P<0.001), and body weight (62.6±9.4 kg vs. 61.8±10.1 kg, P<0.01) were higher in the SD era than in the pre-SD era. Total physical activity was lower in the SD era (2,584.6±2,624.1 MET-min/week–1 vs. 1,987.3±2,295.0 MET-min/week–1, P<0.001). A larger increase in HbA1c level was associated with increased body weight and decreased physical activity.
Conclusion
SD had negative effects on diabetes management in older adults with diabetes. Fasting glucose and HbA1c levels and body weight increased during the SD era. Participants with reduced physical activity gained more weight and had higher blood glucose levels. Given that the COVID-19 pandemic is ongoing, health professionals and diabetes educators should monitor changes in lifestyle factors in older adults with diabetes. -
Citations
Citations to this article as recorded by- Preliminary efficacy of a technology-based physical activity intervention for older Korean adults during the COVID-19 pandemic
Soonhyung Kwon, Oejin Shin, Rosalba Hernandez
Educational Gerontology.2024; 50(1): 27. CrossRef - Obesity and weight change during the COVID‐19 pandemic in children and adults: A systematic review and meta‐analysis
Laura N. Anderson, Yulika Yoshida‐Montezuma, Nora Dewart, Ezza Jalil, Jayati Khattar, Vanessa De Rubeis, Sarah Carsley, Lauren E. Griffith, Lawrence Mbuagbaw
Obesity Reviews.2023;[Epub] CrossRef - Changes in lifestyle-related behaviour during the COVID-19 pandemic in Japan: a questionnaire survey for examinees who underwent an annual health check-up
Miyako Kishimoto, Kayo Masuko, Sumie Yamamoto, Retsu Fujita, Shoko Nakamura, Masato Odawara, Mikio Zeniya
Journal of International Medical Research.2023;[Epub] CrossRef - Glycaemic monitoring and control among high-risk patients with type 2 diabetes in Australian general practice during COVID-19
Kirrilee Jane Barlow, Paul P Fahey, Evan Atlantis
Family Medicine and Community Health.2023; 11(3): e002271. CrossRef - Social isolation, loneliness and subsequent risk of major adverse cardiovascular events among individuals with type 2 diabetes mellitus
Yannis Yan Liang, Yilin Chen, Hongliang Feng, Huachen Xue, Yu Nie, Qi-Yong H Ai, Jiacheng Ma, Lulu Yang, Jihui Zhang, Sizhi Ai
General Psychiatry.2023; 36(6): e101153. CrossRef - Stress, Depression, and Unhealthy Behavior Changes among Patients with Diabetes during COVID-19 in Korea
Hae Ran Kim, Jeong-Soon Kim
Healthcare.2022; 10(2): 303. CrossRef - Reply to comment on “Unexpected decline in glycated hemoglobin level after emergency COVID‐19 measures in three robust older Japanese women with prediabetes/mild type 2 diabetes”
Tazuo Okuno, Osamu Iritani, Kumie Kodera, Daisuke Hama, Asami Kane, Kozue Morigaki, Toshio Terai, Norie Maeno, Shigeto Morimoto
Geriatrics & Gerontology International.2022; 22(7): 541. CrossRef - Anxiety, Distress and Stress among Patients with Diabetes during COVID-19 Pandemic: A Systematic Review and Meta-Analysis
Rubén A. García-Lara, José L. Gómez-Urquiza, María José Membrive-Jiménez, Almudena Velando-Soriano, Monserrat E. Granados-Bolivar, José L. Romero-Béjar, Nora Suleiman-Martos
Journal of Personalized Medicine.2022; 12(9): 1412. CrossRef - Prevalence of Depression and Related Factors among Patients with Chronic Disease during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis
Rubén A. García-Lara, Nora Suleiman-Martos, María J. Membrive-Jiménez, Victoria García-Morales, Miguel Quesada-Caballero, Isabel M. Guisado-Requena, José L. Gómez-Urquiza
Diagnostics.2022; 12(12): 3094. CrossRef
- Preliminary efficacy of a technology-based physical activity intervention for older Korean adults during the COVID-19 pandemic
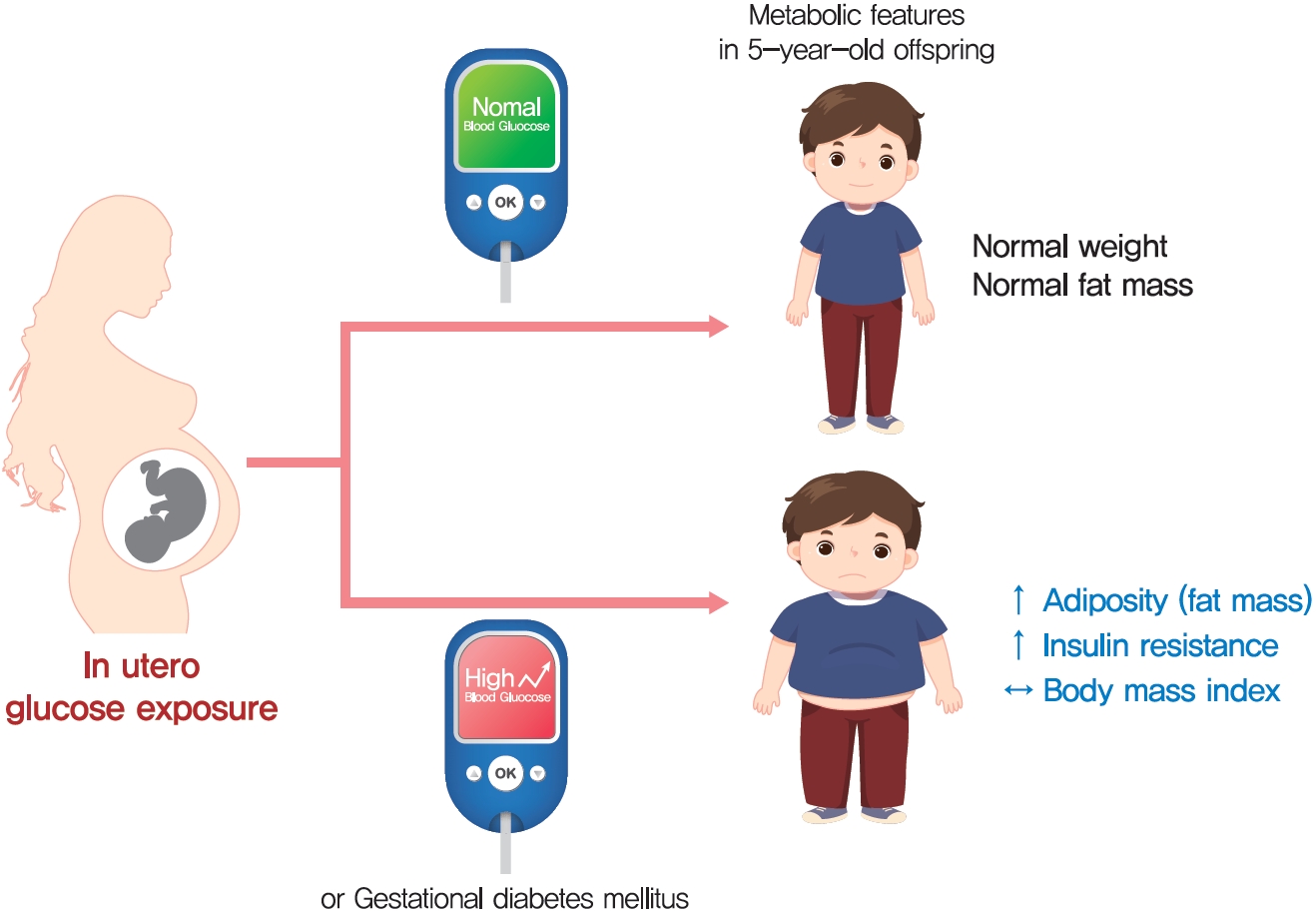
- Metabolic Risk/Epidemiology
- Maternal Hyperglycemia during Pregnancy Increases Adiposity of Offspring
- Hye Rim Chung, Joon Ho Moon, Jung Sub Lim, Young Ah Lee, Choong Ho Shin, Joon-Seok Hong, Soo Heon Kwak, Sung Hee Choi, Hak Chul Jang
- Diabetes Metab J. 2021;45(5):730-738. Published online February 22, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0154
- 5,722 View
- 180 Download
- 6 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 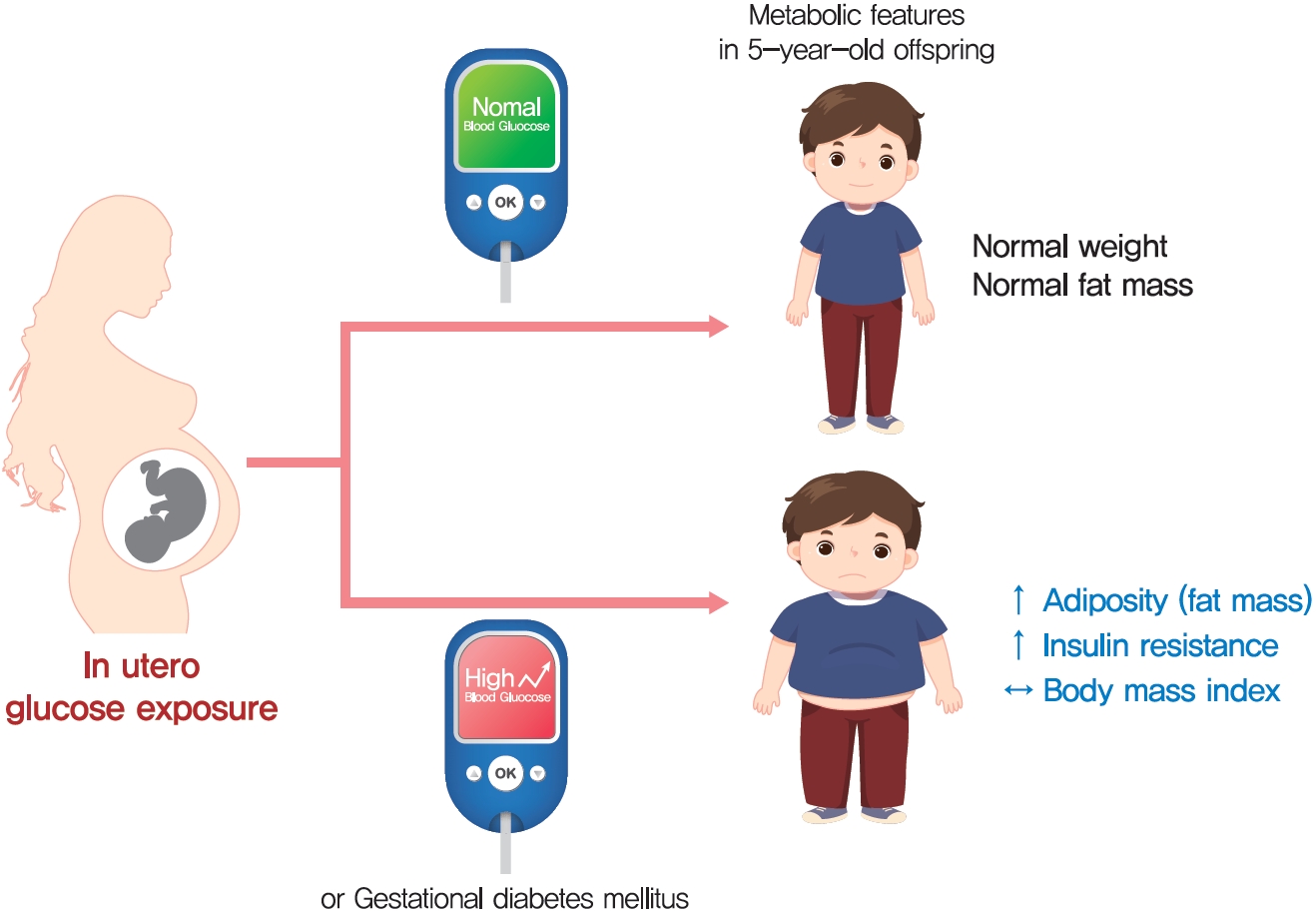
- Background
The effect of intrauterine hyperglycemia on fat mass and regional fat proportion of the offspring of mothers with gestational diabetes mellitus (OGDM) remains to be determined.
Methods
The body composition of OGDM (n=25) and offspring of normoglycemic mothers (n=49) was compared using dualenergy X-ray absorptiometry at age 5 years. The relationship between maternal glucose concentration during a 100 g oral glucose tolerance test (OGTT) and regional fat mass or proportion was analyzed after adjusting for maternal prepregnancy body mass index (BMI).
Results
BMI was comparable between OGDM and control (median, 16.0 kg/m2 vs. 16.1 kg/m2 ). Total, truncal, and leg fat mass were higher in OGDM compared with control (3,769 g vs. 2,245 g, P=0.004; 1,289 g vs. 870 g, P=0.017; 1,638 g vs. 961 g, P=0.002, respectively), whereas total lean mass was lower in OGDM (15,688 g vs. 16,941 g, P=0.001). Among OGDM, total and truncal fat mass were correlated with fasting and 3-hour glucose concentrations of maternal 100 g OGTT during pregnancy (total fat mass, r=0.49, P=0.018 [fasting], r=0.473, P=0.023 [3-hour]; truncal fat mass, r=0.571, P=0.004 [fasting], r=0.558, P=0.006 [3-hour]), but there was no correlation between OGDM leg fat mass and maternal OGTT during pregnancy. Regional fat indices were not correlated with concurrent maternal 75 g OGTT values.
Conclusion
Intrauterine hyperglycemia is associated with increased fat mass, especially truncal fat, in OGDM aged 5 years. -
Citations
Citations to this article as recorded by- Advances in free fatty acid profiles in gestational diabetes mellitus
Haoyi Du, Danyang Li, Laura Monjowa Molive, Na Wu
Journal of Translational Medicine.2024;[Epub] CrossRef - High-fat diet during pregnancy lowers fetal weight and has a long-lasting adverse effect on brown adipose tissue in the offspring
Mihoko Yamaguchi, Jun Mori, Nozomi Nishida, Satoshi Miyagaki, Yasuhiro Kawabe, Takeshi Ota, Hidechika Morimoto, Yusuke Tsuma, Shota Fukuhara, Takehiro Ogata, Takuro Okamaura, Naoko Nakanishi, Masahide Hamaguchi, Hisakazu Nakajima, Michiaki Fukui, Tomoko I
Journal of Developmental Origins of Health and Disease.2023; 14(2): 261. CrossRef - Prediction of gestational diabetes mellitus in Asian women using machine learning algorithms
Byung Soo Kang, Seon Ui Lee, Subeen Hong, Sae Kyung Choi, Jae Eun Shin, Jeong Ha Wie, Yun Sung Jo, Yeon Hee Kim, Kicheol Kil, Yoo Hyun Chung, Kyunghoon Jung, Hanul Hong, In Yang Park, Hyun Sun Ko
Scientific Reports.2023;[Epub] CrossRef - Effects of early standardized management on the growth trajectory of offspring with gestational diabetes mellitus at 0–5 years old: a preliminary longitudinal study
Bingbing Guo, Jingjing Pei, Yin Xu, Yajie Wang, Xinye Jiang
Scientific Reports.2023;[Epub] CrossRef - Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
Joon Ho Moon, Hak Chul Jang
Diabetes & Metabolism Journal.2022; 46(1): 3. CrossRef - Increased Pro-Inflammatory T Cells, Senescent T Cells, and Immune-Check Point Molecules in the Placentas of Patients With Gestational Diabetes Mellitus
Yea Eun Kang, Hyon-Seung Yi, Min-Kyung Yeo, Jung Tae Kim, Danbit Park, Yewon Jung, Ok Soon Kim, Seong Eun Lee, Ji Min Kim, Kyong Hye Joung, Ju Hee Lee, Bon Jeong Ku, Mina Lee, Hyun Jin Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef
- Advances in free fatty acid profiles in gestational diabetes mellitus
- Clinical Diabetes & Therapeutics
- Effects of Lobeglitazone, a Novel Thiazolidinedione, on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus over 52 Weeks
- Soo Lim, Kyoung Min Kim, Sin Gon Kim, Doo Man Kim, Jeong-Taek Woo, Choon Hee Chung, Kyung Soo Ko, Jeong Hyun Park, Yongsoo Park, Sang Jin Kim, Hak Chul Jang, Dong Seop Choi
- Diabetes Metab J. 2017;41(5):377-385. Published online October 24, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.377
- 4,260 View
- 42 Download
- 19 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this multicenter, randomized, double-blind study was to examine the effect of lobeglitazone, a novel thiazolidinedione, on the changes in bone mineral density (BMD) in patients with type 2 diabetes mellitus.
Methods A 24-week, double-blinded phase was followed by a 28-week, open-label phase, in which the placebo group also started to receive lobeglitazone. A total of 170 patients aged 34 to 76 years were randomly assigned in a 2:1 ratio to receive lobeglitazone 0.5 mg or a matching placebo orally, once daily. BMD was assessed using dual-energy X-ray absorptiometry at week 24 and at the end of the study (week 52).
Results During the double-blinded phase, the femur neck BMD showed decreasing patterns in both groups, without statistical significance (−0.85%±0.36% and −0.78%±0.46% in the lobeglitazone and placebo groups, respectively). The treatment difference between the groups was 0.07%, which was also not statistically significant. Further, minimal, nonsignificant decreases were observed in both groups in the total hip BMD compared to values at baseline, and these differences also did not significantly differ between the groups. During the open-label phase, the BMD was further decreased, but not significantly, by −0.32% at the femur neck and by −0.60% at the total hip in the lobeglitazone group, and these changes did not significantly differ compared with the original placebo group switched to lobeglitazone.
Conclusion Our results indicate that treatment with lobeglitazone 0.5 mg over 52 weeks showed no detrimental effect on the BMD compared to the placebo.
-
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - The benefits of adipocyte metabolism in bone health and regeneration
Lisa-Marie Burkhardt, Christian H. Bucher, Julia Löffler, Charlotte Rinne, Georg N. Duda, Sven Geissler, Tim J. Schulz, Katharina Schmidt-Bleek
Frontiers in Cell and Developmental Biology.2023;[Epub] CrossRef - Will lobeglitazone rival pioglitazone? A systematic review and critical appraisal
Kalyan Kumar Gangopadhyay, Awadhesh Kumar Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(4): 102747. CrossRef - Comparison of therapeutic efficacy and safety of sitagliptin, dapagliflozin, or lobeglitazone adjunct therapy in patients with type 2 diabetes mellitus inadequately controlled on sulfonylurea and metformin: Third agent study
Jun Hwa Hong, Jun Sung Moon, Kayeon Seong, Soo Lim
Diabetes Research and Clinical Practice.2023; 203: 110872. CrossRef - Bone Mineral Density Evaluation Among Type 2 Diabetic Patients in Rural Haryana, India: An Analytical Cross-Sectional Study
Nitish Khandelwal, Surbhi Rajauria, Siddhesh Pandurang Kanjalkar, Omkar Shivaji Chavanke, Sanjay Rai
Cureus.2023;[Epub] CrossRef - Lobeglitazone and Its Therapeutic Benefits: A Review
Balamurugan M, Sarumathy S, Robinson R
Cureus.2023;[Epub] CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Y
Diabetes & Metabolism Journal.2022; 46(6): 855. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Lobeglitazone: A Novel Thiazolidinedione for the Management of Type 2 Diabetes Mellitus
Jaehyun Bae, Taegyun Park, Hyeyoung Kim, Minyoung Lee, Bong-Soo Cha
Diabetes & Metabolism Journal.2021; 45(3): 326. CrossRef - Effect of lobeglitazone on motor function in rat model of Parkinson’s disease with diabetes co-morbidity
Kambiz Hassanzadeh, Arman Rahimmi, Mohammad Raman Moloudi, Rita Maccarone, Massimo Corbo, Esmael Izadpanah, Marco Feligioni
Brain Research Bulletin.2021; 173: 184. CrossRef - Recent Perspective on Thiazolidinedione
Won Jun Kim
The Journal of Korean Diabetes.2021; 22(2): 97. CrossRef - Use of in vitro bone models to screen for altered bone metabolism, osteopathies, and fracture healing: challenges of complex models
Sabrina Ehnert, Helen Rinderknecht, Romina H. Aspera-Werz, Victor Häussling, Andreas K. Nussler
Archives of Toxicology.2020; 94(12): 3937. CrossRef - Update on: effects of anti-diabetic drugs on bone metabolism
Guillaume Mabilleau, Béatrice Bouvard
Expert Review of Endocrinology & Metabolism.2020; 15(6): 415. CrossRef - The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: Systematic review and meta‐analysis of observational studies
Khemayanto Hidayat, Xuan Du, Meng‐Jiao Wu, Bi‐Min Shi
Obesity Reviews.2019; 20(10): 1494. CrossRef - Diabetes pharmacotherapy and effects on the musculoskeletal system
Evangelia Kalaitzoglou, John L. Fowlkes, Iuliana Popescu, Kathryn M. Thrailkill
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef - Morin Exerts Anti‐Arthritic Effects by Attenuating Synovial Angiogenesis via Activation of Peroxisome Proliferator Activated Receptor‐γ
Mengfan Yue, Ni Zeng, Yufeng Xia, Zhifeng Wei, Yue Dai
Molecular Nutrition & Food Research.2018;[Epub] CrossRef - The effects of diabetes therapy on bone: A clinical perspective
Karim G. Kheniser, Carmen M. Polanco Santos, Sangeeta R. Kashyap
Journal of Diabetes and its Complications.2018; 32(7): 713. CrossRef - Changes in the Bone Mineral Density of Femur Neck and Total Hip Over a 52-Week Treatment with Lobeglitazone
Da Young Lee, Ji A Seo
Diabetes & Metabolism Journal.2017; 41(5): 374. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
- Clinical Care/Education
- Comparison of Antidiabetic Regimens in Patients with Type 2 Diabetes Uncontrolled by Combination Therapy of Sulfonylurea and Metformin: Results of the MOHAS Disease Registry in Korea
- Sung Hee Choi, Tae Jung Oh, Hak Chul Jang
- Diabetes Metab J. 2017;41(3):170-178. Published online May 11, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.3.170
- 3,569 View
- 35 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the glucose-lowering efficacy of antidiabetic treatments in patients with type 2 diabetes mellitus (T2DM) uncontrolled by sulfonylurea plus metformin.
Methods This open-label, multicenter, prospective, observational study was conducted in 144 centers in Korea, from June 2008 to July 2010, and included patients with T2DM who had received sulfonylurea and metformin for at least 3 months and had levels of glycosylated hemoglobin (HbA1c) >7.0% in the last month. Data of clinical and biochemical characteristics were collected at baseline and 6 months after treatment. The treatment option was decided at the physician's discretion. Subjects were classified into the following three groups: intensifying oral hypoglycemic agents (group A), adding basal insulin (group B), or starting intensified insulin therapy (group C).
Results Of 2,995 patients enrolled, 2,901 patients were evaluated, and 504 (17.4%), 2,316 (79.8%), and 81 patients (2.8%) were classified into groups A, B, and C, respectively. Subjects in group C showed relatively higher baseline levels of HbA1c and longer duration of diabetes. The mean decrease in HbA1c level was higher in the insulin treated groups (−0.9%±1.3%, −1.6%±1.3%, and −2.4%±2.3% in groups A, B, and C, respectively,
P =0.042). The proportion of patients who achieved target HbA1c <7.0% was comparable among the groups; however, intensified insulin therapy seemed to be the most effective in achieving the target HbA1c of 6.5%.Conclusion These findings suggest that insulin-based therapy will be an important option in the improved management of Korean patients with T2DM whose glycemic control is not sufficient with sulfonylurea and metformin.
-
Citations
Citations to this article as recorded by- Metformin-Insulin versus Metformin-Sulfonylurea Combination Therapies in Type 2 Diabetes: A Comparative Study of Glycemic Control and Risk of Cardiovascular Diseases in Addis Ababa, Ethiopia
Desye Gebrie, Tsegahun Manyazewal, Dawit A Ejigu, Eyasu Makonnen
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 3345. CrossRef - Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2017; 41(5): 367. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Insulin therapy for adult patients with type 2 diabetes mellitus: a position statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
The Korean Journal of Internal Medicine.2017; 32(6): 967. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - Insulin
Reactions Weekly.2017; 1665(1): 159. CrossRef
- Metformin-Insulin versus Metformin-Sulfonylurea Combination Therapies in Type 2 Diabetes: A Comparative Study of Glycemic Control and Risk of Cardiovascular Diseases in Addis Ababa, Ethiopia
- Epidemiology
- Application of the 2013 American College of Cardiology/American Heart Association Cholesterol Guideline to the Korean National Health and Nutrition Examination Surveys from 1998 to 2012
- Young Shin Song, Tae Jung Oh, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang, Kyong Soo Park, Soo Lim
- Diabetes Metab J. 2017;41(1):38-50. Published online December 16, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.38
- 4,270 View
- 29 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background The 2013 American College of Cardiology/American Heart Association (ACC/AHA) guideline for the treatment of blood cholesterol recommends statin therapy for individuals at high risk of atherosclerotic cardiovascular disease (ASCVD). The aim of this study was to investigate serial trends in the percentages of Korean adults considered eligible for statin therapy according to the new ACC/AHA cholesterol guideline.
Methods Data from the Korean National Health and Nutrition Examination Survey (KNHANES) I (1998,
n =7,698), II (2001,n =5,654), III (2005,n =5,269), IV (2007 to 2009,n =15,727), and V (2010 to 2012,n =16,304), which used a stratified, multistage, probability sampling design, were used as representative of the entire Korean population.Results The percentage of adults eligible for statin therapy according to the ACC/AHA cholesterol guideline increased with time: 17.0%, 19.0%, 20.8%, 20.2%, and 22.0% in KNHANES I, II, III, IV, and V, respectively (
P =0.022). The prevalence of ASCVD was 1.4% in KNHANES I and increased to 3.3% in KNHANES V. The percentage of diabetic patients aged 40 to 75 years with a low density lipoprotein cholesterol levels of 70 to 189 mg/dL increased from 4.8% in KNHANES I to 6.1% in KNHANES V. People with an estimated 10-year ASCVD risk ≥7.5% and aged 40 to 75 years accounted for the largest percentage among the four statin benefit groups: 9.1% in KNHANES I and 11.0% in KNHANES V.Conclusion Application of the 2013 ACC/AHA guideline has found that the percentage of Korean adults in the statin benefit groups has increased over the past 15 years.
-
Citations
Citations to this article as recorded by- Sex differences in risk factors for subclinical hypothyroidism
Jeonghoon Ha, Jeongmin Lee, Kwanhoon Jo, Dong-Jun Lim, Moo Il Kang, Bong Yun Cha, Min-Hee Kim
Endocrine Connections.2018; 7(4): 511. CrossRef
- Sex differences in risk factors for subclinical hypothyroidism
- Response: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (
Diabetes Metab J 2016;40:140-6) - Ji Won Yoon, Hak Chul Jang
- Diabetes Metab J. 2016;40(3):250-251. Published online June 20, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.250
- 3,187 View
- 29 Download
- 4 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- Muscle Quality in Older Adults: A Scoping Review
Charles Phillipe de Lucena Alves, Samuel Brito de Almeida, Danielle Pessoa Lima, Pedro Braga Neto, Ana Lúcia Miranda, Todd Manini, Lara Vlietstra, Debra L. Waters, Renata Moraes Bielemann, Rosaly Correa-de-Araujo, Ana Paula Fayh, Eduardo Caldas Costa
Journal of the American Medical Directors Association.2023; 24(4): 462. CrossRef - Neuromuscular dysfunction and exercise training in people with diabetic peripheral neuropathy: A narrative review
Giorgio Orlando, Stefano Balducci, Andrew J.M. Boulton, Hans Degens, Neil D. Reeves
Diabetes Research and Clinical Practice.2022; 183: 109183. CrossRef - DPP4 inhibitors as a potential therapeutic option for sarcopenia: A 6-month follow-up study in diabetic older patients
Canberk Sencan, Fatma Sena Dost, Esra Ates Bulut, Ahmet Turan Isik
Experimental Gerontology.2022; 164: 111832. CrossRef - Níveis glicêmicos e sarcopenia em idosos com diabetes mellitus do tipo 2
Isabella Stoeterau, Deise Regina Baptista, Andrea Pires Muller, Juliana Ceronato, Magda Rosa Ramos da Cruz, Carla Viana Dendasck
Revista Científica Multidisciplinar Núcleo do Conhecimento.2022; : 53. CrossRef
- Muscle Quality in Older Adults: A Scoping Review
- Clinical Care/Education
- Sarcopenia, Frailty, and Diabetes in Older Adults
- Hak Chul Jang
- Diabetes Metab J. 2016;40(3):182-189. Published online April 20, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.182
- 6,259 View
- 140 Download
- 77 Web of Science
- 75 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Populations are aging and the prevalence of diabetes mellitus is increasing tremendously. The number of older people with diabetes is increasing unexpectedly. Aging and diabetes are both risk factors for functional disability. Thus, increasing numbers of frail or disabled older patients with diabetes will increase both direct and indirect health-related costs. Diabetes has been reported as an important risk factor of developing physical disability in older adults. Older people with diabetes have lower muscle mass and weaker muscle strength. In addition, muscle quality is poorer in diabetic patients. Sarcopenia and frailty have a common soil and may share a similar pathway for multiple pathologic processes in older people. Sarcopenia is thought to be an intermediate step in the development of frailty in patients with diabetes. Thus, early detection of sarcopenia and frailty in older adults with diabetes should be routine clinical practice to prevent frailty or to intervene earlier in frail patients.
-
Citations
Citations to this article as recorded by- Glycemic control and prescription profiles in internal medicine inpatients: The role of frailty
Jose Carlos Arévalo Lorido, Juana Carretero Gomez, Patricia Vazquez Rodriguez, Ricardo Gómez Huelgas, Carmen Marín Silvente, Fernando Javier Sánchez Lora, Elena Isaba Ares, Anna Pardo i Pelegrín, Onán Pérez Hernández, Javier Ena
European Journal of Internal Medicine.2024; 121: 103. CrossRef - Prolonged hospitalization and 1-year mortality are associated with sarcopenia and malnutrition in older patients with type 2 diabetes: A prospective cohort study
Mileni Vanti Beretta, Tatiana Pedroso de Paula, Ticiana da Costa Rodrigues, Thais Steemburgo
Diabetes Research and Clinical Practice.2024; 207: 111063. CrossRef - Effect of Frailty on Depression among Patients with Late-life Depression: A Test of Anger, Anxiety, and Resilience as Mediators
Junhyung Kim, Hyun-Ghang Jeong, Moon-Soo Lee, Chi-Un Pae, Ashwin A. Patkar, Sang Won Jeon, Cheolmin Shin, Changsu Han
Clinical Psychopharmacology and Neuroscience.2024; 22(2): 253. CrossRef - Urgent needs of caregiving in ageing populations with Alzheimer’s disease and other chronic conditions: Support our loved ones
John W. Culberson, Jonathan Kopel, Ujala Sehar, P. Hemachandra Reddy
Ageing Research Reviews.2023; 90: 102001. CrossRef - Hand grip strength: A reliable assessment tool of frailty status on the person with type 2 diabetes mellitus
Diogo Ramalho, Leonor Silva, Catarina Almeida, Luís Rocha, Gustavo Rocha, Rafaela Veríssimo
Nutrition Clinique et Métabolisme.2023; 37(1): 45. CrossRef - Comprehensive review: Frailty in pancreas transplant candidates and recipients
Ronald F. Parsons, Ekamol Tantisattamo, Wisit Cheungpasitporn, Arpita Basu, Yee Lu, Krista L. Lentine, Kenneth J. Woodside, Neeraj Singh, Joseph Scalea, Tarek Alhamad, Ty B. Dunn, Franco H. Cabeza Rivera, Sandesh Parajuli, Martha Pavlakis, Matthew Cooper
Clinical Transplantation.2023;[Epub] CrossRef - Development and validation of a risk prediction model for frailty in patients with diabetes
Fan Bu, Xiao-hui Deng, Na-ni Zhan, Hongtao Cheng, Zi-lin Wang, Li Tang, Yu Zhao, Qi-yuan Lyu
BMC Geriatrics.2023;[Epub] CrossRef - Amino Acid Profiles in Older Adults with Frailty: Secondary Analysis from MetaboFrail and BIOSPHERE Studies
Riccardo Calvani, Anna Picca, Leocadio Rodriguez-Mañas, Matteo Tosato, Hélio José Coelho-Júnior, Alessandra Biancolillo, Olga Laosa, Jacopo Gervasoni, Aniello Primiano, Lavinia Santucci, Ottavia Giampaoli, Isabelle Bourdel-Marchasson, Sophie C. Regueme, A
Metabolites.2023; 13(4): 542. CrossRef - Where to Start? Physical Assessment, Readiness, and Exercise Recommendations for People With Type 1 or Type 2 Diabetes
Marni Armstrong, Sheri R. Colberg, Ronald J. Sigal
Diabetes Spectrum.2023; 36(2): 105. CrossRef - The Association Between Sarcopenia and Diabetes: From Pathophysiology Mechanism to Therapeutic Strategy
Huiling Chen, Xiaojing Huang, Meiyuan Dong, Song Wen, Ligang Zhou, Xinlu Yuan
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1541. CrossRef - Analysis of Individual Components of Frailty in Simultaneous Pancreas and Kidney, and Solitary Pancreas Transplant Recipients
Sandesh Parajuli, Jon Odorico, Isabel Breyer, Emily Zona, Fahad Aziz, Heather Lorden, Jacqueline Garonzik-Wang, Dixon Kaufman, Didier Mandelbrot
Transplantation Direct.2023; 9(9): e1523. CrossRef - Effects of moderate exercise versus light exercise on fasting blood glucose in obese patients with type 2 diabetes mellitus
Manal Kamel Youssef
Physiotherapy Quarterly.2023; 31(3): 101. CrossRef - Risk factors associated with frailty in older adults with type 2 diabetes: A cross‐sectional study
Chia‐Ling Lin, Neng‐Chun Yu, Hsueh‐Ching Wu, Yuan‐Ching Liu
Journal of Clinical Nursing.2022; 31(7-8): 967. CrossRef - Sarcopenia in patients with multiple sclerosis
Hatice Yuksel, Mehtap Balaban, Ozlem Ozturk Tan, Semra Mungan
Multiple Sclerosis and Related Disorders.2022; 58: 103471. CrossRef - Amino acid profile of skeletal muscle loss in type 2 diabetes: Results from a 7-year longitudinal study in asians
Serena Low, Jiexun Wang, Angela Moh, Su Fen Ang, Keven Ang, Yi-Ming Shao, Jianhong Ching, Hai Ning Wee, Lye Siang Lee, Jean-Paul Kovalik, Wern Ee Tang, Ziliang Lim, Tavintharan Subramaniam, Chee Fang Sum, Su Chi Lim
Diabetes Research and Clinical Practice.2022; 186: 109803. CrossRef - Assessment of Muscle Quantity, Quality and Function
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2022; 31(1): 9. CrossRef - Sarcopenia is associated with cardiovascular risk in men with COPD, independent of adiposity
Ah Young Leem, Young Sam Kim, Kung Soo Chung, Moo Suk Park, Young Ae Kang, Young-Mok Park, Ji Ye Jung
Respiratory Research.2022;[Epub] CrossRef - Decline in skeletal muscle mass is associated with cognitive decline in type 2 diabetes mellitus
Serena Low, Kiat Sern Goh, Tze Pin Ng, Angela Moh, Su Fen Ang, Jonathon Khoo, Keven Ang, Philip Yap, Chin Yee Cheong, Wern Ee Tang, Ziliang Lim, Tavintharan Subramaniam, Chee Fang Sum, Su Chi Lim
Journal of Diabetes and its Complications.2022; 36(9): 108258. CrossRef - Frailty and diabetes in older adults: Overview of current controversies and challenges in clinical practice
Mohd Zaquan Arif Abd.Ghafar, Mark O’Donovan, Duygu Sezgin, Elizabeth Moloney, Ángel Rodríguez-Laso, Aaron Liew, Rónán O’Caoimh
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - Implications of the Metabolic Control of Diabetes in Patients with Frailty Syndrome
Marta Muszalik, Hubert Stępień, Grażyna Puto, Mateusz Cybulski, Donata Kurpas
International Journal of Environmental Research and Public Health.2022; 19(16): 10327. CrossRef - Protective Effect of Delta-Like 1 Homolog Against Muscular Atrophy in a Mouse Model
Ji Young Lee, Minyoung Lee, Dong-Hee Lee, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
Endocrinology and Metabolism.2022; 37(4): 684. CrossRef - Diabetes and osteoporosis – Treating two entities: A challenge or cause for concern?
Nicklas H. Rasmussen, Peter Vestergaard
Best Practice & Research Clinical Rheumatology.2022; 36(3): 101779. CrossRef - Predictors associated with prefrailty in older Taiwanese individuals with type 2 diabetes
Shu-Fen Lee, Chih-Ping Li, Yen-Lin Chen, Dee Pei
Medicine.2022; 101(38): e30432. CrossRef - Association of walking speed with cognitive function in Chinese older adults: A nationally representative cohort study
Jianping Liu, Kaiwang Cui, Qian Chen, Zhiteng Li, Jing Fu, Xiangwen Gong, Hui Xu
Frontiers in Aging Neuroscience.2022;[Epub] CrossRef - Lower insulin level is associated with sarcopenia in community-dwelling frail and non-frail older adults
Yanxia Lu, Wee Shiong Lim, Xia Jin, Ma Schwe Zin Nyunt, Tamas Fulop, Qi Gao, Su Chi Lim, Anis Larbi, Tze Pin Ng
Frontiers in Medicine.2022;[Epub] CrossRef - Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults
Nam Hoon Kim, Yousung Park, Nan Hee Kim, Sin Gon Kim
Age and Ageing.2021; 50(3): 780. CrossRef - Examining the links between regular leisure‐time physical activity, sitting time and prefrailty in community‐dwelling older adults
Shu‐Hung Chang, Nai‐Hui Chien, Jackson Pui‐Man Wai, Ching‐Cheng Chiang, Ching‐Yi Yu
Journal of Advanced Nursing.2021; 77(6): 2761. CrossRef - Tale of the Frail: Understanding Frailty in Cirrhosis
Faruq Pradhan, Natasha Narang, Michael Fallon
Southern Medical Journal.2021; 114(3): 186. CrossRef - Type 2 diabetes mellitus in older adults: clinical considerations and management
Srikanth Bellary, Ioannis Kyrou, James E. Brown, Clifford J. Bailey
Nature Reviews Endocrinology.2021; 17(9): 534. CrossRef - Low Protein Intakes and Poor Diet Quality Associate with Functional Limitations in US Adults with Diabetes: A 2005–2016 NHANES Analysis
Stephanie M. Fanelli, Owen J. Kelly, Jessica L. Krok-Schoen, Christopher A. Taylor
Nutrients.2021; 13(8): 2582. CrossRef - Yaşlı Diyabetik Hastalarda Malnutrisyonun Klinik Sonuçları ve Önemi
Saadet KOÇ OKUDUR, Pinar SOYSAL
OSMANGAZİ JOURNAL OF MEDICINE.2021;[Epub] CrossRef - Combined Aerobic and Resistance Exercise Training Reduces Circulating Apolipoprotein J Levels and Improves Insulin Resistance in Postmenopausal Diabetic Women
Yun Kyung Jeon, Sang Soo Kim, Jong Ho Kim, Hyun Jeong Kim, Hyun Jun Kim, Jang Jun Park, Yuen Suk Cho, So Hee Joung, Ji Ryang Kim, Bo Hyun Kim, Sang Heon Song, In Joo Kim, Yong Ki Kim, Young-Bum Kim
Diabetes & Metabolism Journal.2020; 44(1): 103. CrossRef - Effects of elastic band exercise on the frailty states in pre-frail elderly people
Rujie Chen, Qingwen Wu, Dongyan Wang, Zhou Li, Howe Liu, Guangtian Liu, Ying Cui, Linlin Song
Physiotherapy Theory and Practice.2020; 36(9): 1000. CrossRef - Association between Lower Extremity Skeletal Muscle Mass and Impaired Cognitive Function in Type 2 Diabetes
Serena Low, Tze Pin Ng, Chin Leong Lim, Angela Moh, Su Fen Ang, Jiexun Wang, Kiat Sern Goh, Keven Ang, Wern Ee Tang, Pek Yee Kwan, Tavintharan Subramaniam, Chee Fang Sum, Su Chi Lim
Scientific Reports.2020;[Epub] CrossRef - Low free triiodothyronine levels are associated with risk of frailty in older adults with type 2 diabetes mellitus
Shuangling Xiu, Zhijing Mu, Lei Zhao, Lina Sun
Experimental Gerontology.2020; 138: 111013. CrossRef - The Biomechanics of Diabetes Mellitus and Limb Preservation
Jonathan M. Labovitz, Dana Day
Clinics in Podiatric Medicine and Surgery.2020; 37(1): 151. CrossRef - Inorganic Arsenic Exposure Decreases Muscle Mass and Enhances Denervation-Induced Muscle Atrophy in Mice
Chang-Mu Chen, Min-Ni Chung, Chen-Yuan Chiu, Shing-Hwa Liu, Kuo-Cheng Lan
Molecules.2020; 25(13): 3057. CrossRef - Physical Exercise and Myokines: Relationships with Sarcopenia and Cardiovascular Complications
Sandra Maria Barbalho, Uri Adrian Prync Flato, Ricardo José Tofano, Ricardo de Alvares Goulart, Elen Landgraf Guiguer, Cláudia Rucco P. Detregiachi, Daniela Vieira Buchaim, Adriano Cressoni Araújo, Rogério Leone Buchaim, Fábio Tadeu Rodrigues Reina, Piero
International Journal of Molecular Sciences.2020; 21(10): 3607. CrossRef - The relationships between sarcopenic skeletal muscle loss during ageing and macronutrient metabolism, obesity and onset of diabetes
Ailsa A. Welch, Richard P. G. Hayhoe, Donnie Cameron
Proceedings of the Nutrition Society.2020; 79(1): 158. CrossRef - Effects of low skeletal muscle mass and sarcopenic obesity on albuminuria: a 7-year longitudinal study
Jee Hee Yoo, Gyuri Kim, Sung Woon Park, Min Sun Choi, Jiyeon Ahn, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Mira Kang, Jae Hyeon Kim
Scientific Reports.2020;[Epub] CrossRef - Sarcopenia, nutritional status and type 2 diabetes mellitus: A cross‐sectional study in a group of Mexican women residing in a nursing home
María C. Velázquez‐Alva, María E. Irigoyen‐Camacho, Marco A. Zepeda‐Zepeda, Irina Lazarevich, Isabel Arrieta‐Cruz, Carlos D'Hyver
Nutrition & Dietetics.2020; 77(5): 515. CrossRef - Assessing the association between optimal energy intake and all‐cause mortality in older patients with diabetes mellitus using the Japanese Elderly Diabetes Intervention Trial
Takuya Omura, Yoshiaki Tamura, Takuya Yamaoka, Yukio Yoshimura, Takashi Sakurai, Hiroyuki Umegaki, Chiemi Kamada, Satoshi Iimuro, Yasuo Ohashi, Hideki Ito, Atsushi Araki
Geriatrics & Gerontology International.2020; 20(1): 59. CrossRef - Sarkopenie im Kontext von Insulinresistenz und Diabetes mellitus im Alter – Daten aus der Berliner Altersstudie II
Dominik Spira, Nikolaus Buchmann, Knut Mai, Thomas Bobbert, Joachim Spranger, Ilja Demuth, Elisabeth Steinhagen-Thiessen
Diabetologie und Stoffwechsel.2020; 15(05): 400. CrossRef - Effect of Dietary Silk Peptide on Obesity, Hyperglycemia, and Skeletal Muscle Regeneration in High-Fat Diet-Fed Mice
Kippeum Lee, Heegu Jin, Sungwoo Chei, Hyun-Ji Oh, Jeong-Yong Lee, Boo-Yong Lee
Cells.2020; 9(2): 377. CrossRef - Nutrition Management in Older Adults with Diabetes: A Review on the Importance of Shifting Prevention Strategies from Metabolic Syndrome to Frailty
Yoshiaki Tamura, Takuya Omura, Kenji Toyoshima, Atsushi Araki
Nutrients.2020; 12(11): 3367. CrossRef - Mechanical Properties of Single Muscle Fibers: Understanding Poor Muscle Quality in Older Adults with Diabetes
Eun-Jeong Lee, Hak Chul Jang, Kyung-Hoi Koo, Hye-Young Kim, Jae-Young Lim
Annals of Geriatric Medicine and Research.2020; 24(4): 267. CrossRef - Mortality is not increased with Diabetes in hospitalised very old adults: a multi-site review
Peter Smerdely
BMC Geriatrics.2020;[Epub] CrossRef - Falls and Fractures in Diabetes—More than Bone Fragility
Nicklas Højgaard Rasmussen, Jakob Dal
Current Osteoporosis Reports.2019; 17(3): 147. CrossRef - Measuring gait speed to better identify prodromal dementia
Giulia Grande, Federico Triolo, Arturo Nuara, Anna-Karin Welmer, Laura Fratiglioni, Davide L. Vetrano
Experimental Gerontology.2019; 124: 110625. CrossRef - Diabetes and Muscle Dysfunction in Older Adults
Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 160. CrossRef - Association between sarcopenia and diabetes in community dwelling elderly in the Amazon region – Viver Mais Project
Anelza Biene Farias Souza, David Anchieta Costa Nascimento, Isabella Juliana Manfredo Rodrigues, Cynthia Cillene Oliveira Charone, Geovanna Lemos Lopes, Rondinei Silva Lima, Ana Amália Sá, Thiago Xavier Carneiro, Niele Silva Moraes
Archives of Gerontology and Geriatrics.2019; 83: 121. CrossRef - Association between deterioration in muscle strength and peripheral neuropathy in people with diabetes
Tae Jung Oh, Sunyoung Kang, Jie-Eun Lee, Jae Hoon Moon, Sung Hee Choi, Soo Lim, Hak Chul Jang
Journal of Diabetes and its Complications.2019; 33(8): 598. CrossRef - Frailty and Disability in Diabetes
Sol-Ji Yoon, Kwang-il Kim
Annals of Geriatric Medicine and Research.2019; 23(4): 165. CrossRef - Mechanisms Involved in Glycemic Control Promoted by Exercise in Diabetics
Eric Francelino Andrade, Víviam de Oliveira Silva, Débora Ribeiro Orlando, Luciano José Pereira
Current Diabetes Reviews.2019; 15(2): 105. CrossRef - Response: The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity (J Obes Metab Syndr 2019;28:46-52)
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 297. CrossRef - Diabetic Peripheral Neuropathy as a Risk Factor for Sarcopenia
Tae Jung Oh, Yoojung Song, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 170. CrossRef - Sarcopenia and hospital-related outcomes in the old people: a systematic review and meta-analysis
Yunli Zhao, Yunxia Zhang, Qiukui Hao, Meiling Ge, Birong Dong
Aging Clinical and Experimental Research.2019; 31(1): 5. CrossRef - The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(1): 46. CrossRef - Sarcopenia in elderly patients with type 2 diabetes mellitus: prevalence and related clinical factors
Yuko Murata, Yoshiki Kadoya, Shoichi Yamada, Tokio Sanke
Diabetology International.2018; 9(2): 136. CrossRef - Assessment of lower extremity muscle mass, muscle strength, and exercise therapy in elderly patients with diabetes mellitus
Takuo Nomura, Toshihiro Kawae, Hiroaki Kataoka, Yukio Ikeda
Environmental Health and Preventive Medicine.2018;[Epub] CrossRef - Diabetes Treatment in the Elderly: Incorporating Geriatrics, Technology, and Functional Medicine
Willy Marcos Valencia, Diana Botros, Maria Vera-Nunez, Stuti Dang
Current Diabetes Reports.2018;[Epub] CrossRef - Psoas and paraspinous muscle index as a predictor of mortality in African American men with type 2 diabetes mellitus
Mariana Murea, Leon Lenchik, Thomas C. Register, Gregory B. Russell, Jianzhao Xu, S. Carrie Smith, Donald W. Bowden, Jasmin Divers, Barry I. Freedman
Journal of Diabetes and its Complications.2018; 32(6): 558. CrossRef - Presence of Sarcopenia and Its Rate of Change Are Independently Associated with Long-term Mortality in Patients with Liver Cirrhosis
Jae Yoon Jeong, Sanghyeok Lim, Joo Hyun Sohn, Jae Gon Lee, Dae Won Jun, Yongsoo Kim
Journal of Korean Medical Science.2018;[Epub] CrossRef - Comparison between Dual-Energy X-ray Absorptiometry and Bioelectrical Impedance Analyses for Accuracy in Measuring Whole Body Muscle Mass and Appendicular Skeletal Muscle Mass
Seo Lee, Soyeon Ahn, Young Kim, Myoung Ji, Kyoung Kim, Sung Choi, Hak Jang, Soo Lim
Nutrients.2018; 10(6): 738. CrossRef - The association of low muscle mass with soluble receptor for advanced glycation end products (sRAGE): The Korean Sarcopenic Obesity Study (KSOS)
Tae Nyun Kim, Man Sik Park, Eun Joo Lee, Hye Soo Chung, Hye Jin Yoo, Hyun Joo Kang, Wook Song, Sei Hyun Baik, Kyung Mook Choi
Diabetes/Metabolism Research and Reviews.2018;[Epub] CrossRef - Obesity paradox on the survival of elderly patients with diabetes: an AHAP-based study
Ali Bijani, Robert G. Cumming, Seyed-Reza Hosseini, Masoumeh Yazdanpour, Mahdis Rahimi, Abbas Sahebian, Reza Ghadimi
Journal of Diabetes & Metabolic Disorders.2018; 17(1): 45. CrossRef - Effects of Seahorse Supplementation on Muscle Mass, Exercise Performance Abilities and the Related Blood Factors in Healthy Elderly Women
Bae-jin LEE, Chan-ho PARK, Byeong-Hwan JEON
JOURNAL OF FISHRIES AND MARINE SCIENCES EDUCATION.2018; 30(2): 409. CrossRef - Frailty risk in hospitalised older adults with and without diabetes mellitus
Deborah A. Lekan, Thomas P. McCoy
Journal of Clinical Nursing.2018; 27(19-20): 3510. CrossRef - Sarcopenia
А.А. Пальцын
ZHurnal «Patologicheskaia fiziologiia i eksperimental`naia terapiia».2018; (2()): 113. CrossRef - Prevention of Falls and Frailty in Older Adults with Diabetes
Helen P. Hazuda, Sara E. Espinoza
Current Geriatrics Reports.2017; 6(3): 158. CrossRef - Patterns and Predictors of Frailty Transitions in Older Men: The Osteoporotic Fractures in Men Study
Lauren R. Pollack, Stephanie Litwack‐Harrison, Peggy M. Cawthon, Kristine Ensrud, Nancy E. Lane, Elizabeth Barrett‐Connor, Thuy‐Tien Dam
Journal of the American Geriatrics Society.2017; 65(11): 2473. CrossRef - Diabetic Neuropathy and Gait: A Review
Uazman Alam, David R. Riley, Ravinder S. Jugdey, Shazli Azmi, Satyan Rajbhandari, Kristiaan D’Août, Rayaz A. Malik
Diabetes Therapy.2017; 8(6): 1253. CrossRef - Care of older people with diabetes
Trisha Dunning
Nursing Standard.2017; 32(3): 50. CrossRef - Decreased Muscle Strength and Quality in Diabetes-Related Dementia
Akito Tsugawa, Yusuke Ogawa, Naoto Takenoshita, Yoshitsugu Kaneko, Hirokuni Hatanaka, Eriko Jaime, Raita Fukasawa, Haruo Hanyu
Dementia and Geriatric Cognitive Disorders Extra.2017; 7(3): 454. CrossRef - Aging of the endocrine system and its potential impact on sarcopenia
Giovanni Vitale, Matteo Cesari, Daniela Mari
European Journal of Internal Medicine.2016; 35: 10. CrossRef
- Glycemic control and prescription profiles in internal medicine inpatients: The role of frailty
- Clinical Care/Education
- Feasibility of a Patient-Centered, Smartphone-Based, Diabetes Care System: A Pilot Study
- Eun Ky Kim, Soo Heon Kwak, Seungsu Baek, Seung Lyeol Lee, Hak Chul Jang, Kyong Soo Park, Young Min Cho
- Diabetes Metab J. 2016;40(3):192-201. Published online April 8, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.192
- 5,093 View
- 53 Download
- 20 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We developed a patient-centered, smartphone-based, diabetes care system (PSDCS). This study aims to test the feasibility of glycosylated hemoglobin (HbA1c) reduction with the PSDCS.
Methods This study was a single-arm pilot study. The participants with type 2 diabetes mellitus were instructed to use the PSDCS, which integrates a Bluetooth-connected glucometer, digital food diary, and wearable physical activity monitoring device. The primary end point was the change in HbA1c from baseline after a 12-week intervention.
Results Twenty-nine patients aged 53.9±9.1 years completed the study. HbA1c and fasting plasma glucose levels decreased significantly from baseline (7.7%±0.7% to 7.1%±0.6%,
P <0.0001; 140.9±39.1 to 120.1±31.0 mg/dL,P =0.0088, respectively). The frequency of glucose monitoring correlated with the magnitude of HbA1c reduction (r =–0.57,P =0.0013). The components of the diabetes self-care activities, including diet, exercise, and glucose monitoring, were significantly improved, particularly in the upper tertile of HbA1c reduction. There were no severe adverse events during the intervention.Conclusion A 12-week application of the PSDCS to patients with inadequately controlled type 2 diabetes resulted in a significant HbA1c reduction with tolerable safety profiles; these findings require confirmation in a future randomized controlled trial.
-
Citations
Citations to this article as recorded by- Telehealth Technologies in Diabetes Self-management and Education
Vidya Sharma, Marie Feldman, Ramaswamy Sharma
Journal of Diabetes Science and Technology.2024; 18(1): 148. CrossRef - App Design Features Important for Diabetes Self-management as Determined by the Self-Determination Theory on Motivation: Content Analysis of Survey Responses From Adults Requiring Insulin Therapy
Helen N C Fu, Jean F Wyman, Cynthia J Peden-McAlpine, Claire Burke Draucker, Titus Schleyer, Terrence J Adam
JMIR Diabetes.2023; 8: e38592. CrossRef - The Clinical Impact of Flash Glucose Monitoring—a Digital Health App and Smartwatch Technology in Patients With Type 2 Diabetes: Scoping Review
Sergio Diez Alvarez, Antoni Fellas, Derek Santos, Dean Sculley, Katie Wynne, Shamasunder Acharya, Pooshan Navathe, Xavier Girones, Andrea Coda
JMIR Diabetes.2023; 8: e42389. CrossRef - User Retention and Engagement in the Digital-Based Diabetes Education and Self-Management for Ongoing and Newly Diagnosed (myDESMOND) Program: Descriptive Longitudinal Study
Mary M Barker, Radhika Chauhan, Melanie J Davies, Christopher Brough, Alison Northern, Bernie Stribling, Sally Schreder, Kamlesh Khunti, Michelle Hadjiconstantinou
JMIR Diabetes.2023; 8: e44943. CrossRef - New Digital Health Technologies for Insulin Initiation and Optimization for People With Type 2 Diabetes
David Kerr, Steven Edelman, Giacomo Vespasiani, Kamlesh Khunti
Endocrine Practice.2022; 28(8): 811. CrossRef - Effects of Patient-Driven Lifestyle Modification Using Intermittently Scanned Continuous Glucose Monitoring in Patients With Type 2 Diabetes: Results From the Randomized Open-label PDF Study
Hun Jee Choe, Eun-Jung Rhee, Jong Chul Won, Kyong Soo Park, Won-Young Lee, Young Min Cho
Diabetes Care.2022; 45(10): 2224. CrossRef - Assessing the Acceptability and Effectiveness of Mobile-Based Physical Activity Interventions for Midlife Women During Menopause: Systematic Review of the Literature
Ghada AlSwayied, Haoyue Guo, Tasmin Rookes, Rachael Frost, Fiona L Hamilton
JMIR mHealth and uHealth.2022; 10(12): e40271. CrossRef - Application of the National Institute for Health and Care Excellence Evidence Standards Framework for Digital Health Technologies in Assessing Mobile-Delivered Technologies for the Self-Management of Type 2 Diabetes Mellitus: Scoping Review
Jessica R Forsyth, Hannah Chase, Nia W Roberts, Laura C Armitage, Andrew J Farmer
JMIR Diabetes.2021; 6(1): e23687. CrossRef - Mobile Healthcare System Provided by Primary Care Physicians Improves Quality of Diabetes Care
Tae Jung Oh, Jie-Eun Lee, Seok Kim, Sooyoung Yoo, Hak Chul Jang
CardioMetabolic Syndrome Journal.2021; 1(1): 88. CrossRef - Self-Care IoT Platform for Diabetic Mellitus
Jai-Chang Park, Seongbeom Kim, Je-Hoon Lee
Applied Sciences.2021; 11(5): 2006. CrossRef - Diabetes clinic reinvented: will technology change the future of diabetes care?
Marwa Al-Badri, Osama Hamdy
Therapeutic Advances in Endocrinology and Metabolism.2021; 12: 204201882199536. CrossRef - Analysis of Effectiveness and Psychological Techniques Implemented in mHealth Solutions for Middle-Aged and Elderly Adults with Type 2 Diabetes: A Narrative Review of the Literature
Julia Vázquez-de Sebastián, Andreea Ciudin, Carmina Castellano-Tejedor
Journal of Clinical Medicine.2021; 10(12): 2701. CrossRef - Therapeutic Exercise Platform for Type-2 Diabetic Mellitus
Je-Hoon Lee, Jai-Chang Park, Seong-Beom Kim
Electronics.2021; 10(15): 1820. CrossRef - Accuracy comparison study of new smartphone-based semen analyzer versus laboratory sperm quality analyzer
Min Jung Park, Mi Young Lim, Hyun Jun Park, Nam Cheol Park
Investigative and Clinical Urology.2021; 62(6): 672. CrossRef - User Retention and Engagement With a Mobile App Intervention to Support Self-Management in Australians With Type 1 or Type 2 Diabetes (My Care Hub): Mixed Methods Study
Mary D Adu, Usman H Malabu, Aduli EO Malau-Aduli, Aaron Drovandi, Bunmi S Malau-Aduli
JMIR mHealth and uHealth.2020; 8(6): e17802. CrossRef - The role of telehealth counselling with mobile self-monitoring on blood pressure reduction among overseas Koreans with high blood pressure in Vietnam
Hyang Yuol Lee, Ju Young Kim, Ki Young Na, Hwa Yeon Park, Jinah Han, Yuliya Pak, Bola Nam, Chae Hyun Pae, Jisun Lee, Tae Ho Lim, Donghun Lee
Journal of Telemedicine and Telecare.2019; 25(4): 241. CrossRef - The Effect of a Smartphone-Based, Patient-Centered Diabetes Care System in Patients With Type 2 Diabetes: A Randomized, Controlled Trial for 24 Weeks
Eun Ky Kim, Soo Heon Kwak, Hye Seung Jung, Bo Kyung Koo, Min Kyong Moon, Soo Lim, Hak Chul Jang, Kyong Soo Park, Young Min Cho
Diabetes Care.2019; 42(1): 3. CrossRef - Patient-Driven Diabetes Care of the Future in the Technology Era
Sahar Ashrafzadeh, Osama Hamdy
Cell Metabolism.2019; 29(3): 564. CrossRef - Peripartum Management of Gestational Diabetes Using a Digital Health Care Service: A Pilot, Randomized Controlled Study
Ji-Hee Sung, Da Young Lee, Kyoung Pil Min, Cheol-Young Park
Clinical Therapeutics.2019; 41(11): 2426. CrossRef - The Effects of Dietary Mobile Apps on Nutritional Outcomes in Adults with Chronic Diseases: A Systematic Review and Meta-Analysis
Cosette Fakih El Khoury, Mirey Karavetian, Ruud J.G. Halfens, Rik Crutzen, Lama Khoja, Jos M.G.A. Schols
Journal of the Academy of Nutrition and Dietetics.2019; 119(4): 626. CrossRef - Diabetes Mellitus m-Health Applications: A Systematic Review of Features and Fundamentals
Ericles Andrei Bellei, Daiana Biduski, Nathália Pinto Cechetti, Ana Carolina Bertoletti De Marchi
Telemedicine and e-Health.2018; 24(11): 839. CrossRef - Multifunctional Wearable System that Integrates Sweat‐Based Sensing and Vital‐Sign Monitoring to Estimate Pre‐/Post‐Exercise Glucose Levels
Yongseok Joseph Hong, Hyunjae Lee, Jaemin Kim, Minha Lee, Hyung Jin Choi, Taeghwan Hyeon, Dae‐Hyeong Kim
Advanced Functional Materials.2018;[Epub] CrossRef - Smart Devices for Older Adults Managing Chronic Disease: A Scoping Review
Ben YB Kim, Joon Lee
JMIR mHealth and uHealth.2017; 5(5): e69. CrossRef - Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: A systematic review
Helen Fu, Siobhan K. McMahon, Cynthia R. Gross, Terrence J. Adam, Jean F. Wyman
Diabetes Research and Clinical Practice.2017; 131: 70. CrossRef - Novel device for male infertility screening with single-ball lens microscope and smartphone
Yoshitomo Kobori, Peter Pfanner, Gail S. Prins, Craig Niederberger
Fertility and Sterility.2016; 106(3): 574. CrossRef
- Telehealth Technologies in Diabetes Self-management and Education
- Clinical Care/Education
- Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging
- Ji Won Yoon, Yong-Chan Ha, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Soo Lim, Young Joo Park, Jae Young Lim, Ki Woong Kim, Kyong Soo Park, Hak Chul Jang
- Diabetes Metab J. 2016;40(2):140-146. Published online March 31, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.2.140
- 7,304 View
- 78 Download
- 86 Web of Science
- 89 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The study aimed to investigate the influence of hyperglycemia on muscle quality in older men with type 2 diabetes.
Methods This was a subsidiary study of the Korean Longitudinal Study of Health and Aging. Among 326 older men consenting to tests of body composition and muscle strength, 269 men were ultimately analyzed after the exclusion because of stroke (
n =30) and uncertainty about the diagnosis of diabetes (n =27). Body composition was measured using dual-energy X-ray absorptiometry and computed tomography. Muscle strength for knee extension was measured using an isokinetic dynamometer. Muscle quality was assessed from the ratio of leg strength to the entire corresponding leg muscle mass.Results The muscle mass, strength, and quality in patients with type 2 diabetes did not differ significantly from controls. However, when patients with diabetes were subdivided according to their glycemic control status, patients with a glycosylated hemoglobin (HbA1c) level of ≥8.5% showed significantly decreased leg muscle quality by multivariate analysis (odds ratio, 4.510;
P =0.045) after adjustment for age, body mass index, smoking amount, alcohol consumption, physical activity, and duration of diabetes. Physical performance status was also impaired in subjects with an HbA1c of ≥8.5%.Conclusion Poor glycemic control in these older patients with diabetes was associated with significant risk of decreased muscle quality and performance status. Glycemic control with an HbA1c of <8.5% might be needed to reduce the risk of adverse skeletal and functional outcomes in this population.
-
Citations
Citations to this article as recorded by- Downhill running and caloric restriction attenuate insulin resistance associated skeletal muscle atrophy via the promotion of M2-like macrophages through TRIB3-AKT pathway
Wei Luo, Yue Zhou, Qiang Tang, Yuhang Wang, Yansong Liu, Lei Ai
Free Radical Biology and Medicine.2024; 210: 271. CrossRef - Diabetic Sarcopenia. A proposed muscle screening protocol in people with diabetes
Daniel de Luis Román, Juana Carretero Gómez, José Manuel García-Almeida, Fernando Garrachón Vallo, German Guzmán Rolo, Juan José López Gómez, Francisco José Tarazona-Santabalbina, Alejandro Sanz-Paris
Reviews in Endocrine and Metabolic Disorders.2024;[Epub] CrossRef - Dynapenia and sarcopenia: association with the diagnosis, duration and complication of type 2 diabetes mellitus in ELSA-Brasil
Débora Noara Duarte dos Santos, Carolina Gomes Coelho, Maria de Fátima Haueisen Sander Diniz, Bruce Bartholow Duncan, Maria Inês Schmidt, Isabela Judith Martins Bensenor, Claudia Szlejf, Rosa Weiss Telles, Sandhi Maria Barreto
Cadernos de Saúde Pública.2024;[Epub] CrossRef - Breaking Down Cachexia: A Narrative Review on the Prevalence of Cachexia in Cancer Patients and Its Associated Risk Factors
Mahmathi Karuppannan, Fares M. S. Muthanna, Fazlin Mohd Fauzi
Nutrition and Cancer.2024; 76(5): 404. CrossRef - Mechanism of muscle atrophy in a normal-weight rat model of type 2 diabetes established by using a soft-pellet diet
Sayaka Akieda-Asai, Hao Ma, Wanxin Han, Junko Nagata, Fumitake Yamaguchi, Yukari Date
Scientific Reports.2024;[Epub] CrossRef - Morphological and functional changes in skeletal muscle in type 2 diabetes mellitus: A systematic review and meta-analysis
Jardeson Rocha Filgueiras, Cleudiane Pereira Sales, Ivanilson Gomes da Silva, Cristiana Maria Dos Santos, Elias de Carvalho Magalhães Neto, Rebeca Barbosa da Rocha, Vinicius Saura Cardoso
Physiotherapy Theory and Practice.2023; 39(9): 1789. CrossRef - Hypoglycemic drug liraglutide alleviates low muscle mass by inhibiting the expression of MuRF1 and MAFbx in diabetic muscle atrophy
Dongmei Fan, Yue Wang, Bowei Liu, Fuzai Yin
Journal of the Chinese Medical Association.2023; 86(2): 166. CrossRef - Mechanisms underlying altered neuromuscular function in people with DPN
Antonin Le Corre, Nathan Caron, Nicolas A. Turpin, Georges Dalleau
European Journal of Applied Physiology.2023; 123(7): 1433. CrossRef - Effects of body compositions on the associations between ferritin and diabetes parameters among Japanese community dwellers
Kyi Mar Wai, Rei Akuzawa, Yoko Umeda, Wataru Munakata, Yoshiko Takahashi, Shigeyuki Nakaji, Kazushige Ihara
Journal of Trace Elements in Medicine and Biology.2023; 78: 127174. CrossRef - Effects of glycemic control on frailty: a multidimensional perspective
Ahmed H Abdelhafiz
Hospital Practice.2023; 51(3): 124. CrossRef - Hand grip strength is inversely associated with total daily insulin dose requirement in patients with type 2 diabetes mellitus: a cross-sectional study
Da-shuang Chen, Yun-qing Zhu, Wen-ji Ni, Yu-jiao Li, Guo-ping Yin, Zi-yue Shao, Jian Zhu
PeerJ.2023; 11: e15761. CrossRef - Sarcopenia in Type 2 Diabetes Mellitus: Study of the Modifiable Risk Factors Involved
Surapaneni Lakshmi Sravya, Jayshree Swain, Abhay Kumar Sahoo, Swayamsidha Mangaraj, Jayabhanu Kanwar, Pooja Jadhao, Srijit Das
Journal of Clinical Medicine.2023; 12(17): 5499. CrossRef - Salbutamol ameliorates skeletal muscle wasting and inflammatory markers in streptozotocin (STZ)-induced diabetic rats
Anand Kumar, Priyanka Prajapati, Vinit Raj, Seong-Cheol Kim, Vikas Mishra, Chaitany Jayprakash Raorane, Ritu Raj, Dinesh Kumar, Sapana Kushwaha
International Immunopharmacology.2023; 124: 110883. CrossRef - Decreased serum musclin concentration is independently associated with the high prevalence of sarcopenia in Chinese middle‐elderly patients with type 2 diabetes mellitus
Lei Fu, Qing Zhang, Juan Liu, Xiaoqing Yuan, Xinhua Ye
Journal of Diabetes Investigation.2023; 14(12): 1412. CrossRef - Association between relative muscle strength and hypertension in middle-aged and older Chinese adults
Jin-hua Luo, Tu-ming Zhang, Lin-lin Yang, Yu-ying Cai, Yu Yang
BMC Public Health.2023;[Epub] CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Management of Hyperglycemia in Older Adults with Type 2 Diabetes
Gunjan Y. Gandhi, Arshag D. Mooradian
Drugs & Aging.2022; 39(1): 39. CrossRef - Deleterious Effect of High-Fat Diet on Skeletal Muscle Performance Is Prevented by High-Protein Intake in Adult Rats but Not in Old Rats
Eleonora Poggiogalle, Fanny Rossignon, Aude Carayon, Fréderic Capel, Jean-Paul Rigaudière, Sarah De Saint Vincent, Olivier Le-Bacquer, Jérôme Salles, Christophe Giraudet, Véronique Patrac, Patrice Lebecque, Stéphane Walrand, Yves Boirie, Vincent Martin, C
Frontiers in Physiology.2022;[Epub] CrossRef - Metabolic phenotypes explain the relationship between dysglycaemia and frailty in older people with type 2 diabetes
A.H. Abdelhafiz, A.J. Sinclair
Journal of Diabetes and its Complications.2022; 36(4): 108144. CrossRef - Altered features of body composition in older adults with type 2 diabetes and prediabetes compared with matched controls
Kirsten E. Bell, Michael T. Paris, Egor Avrutin, Marina Mourtzakis
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(2): 1087. CrossRef - A modern approach to glucose-lowering therapy in frail older people with type 2 diabetes mellitus
Ahmed H. Abdelhafiz, Daniel Pennells, Alan J. Sinclair
Expert Review of Endocrinology & Metabolism.2022; 17(2): 95. CrossRef - Metabolic syndrome and its association with components of sarcopenia in older community-dwelling Chinese
Qiangwei Tong, Xiao Wang, Yunlu Sheng, Shu Chen, Bin Lai, Rong Lv, Jing Yu
The Journal of Biomedical Research.2022; 36(2): 120. CrossRef - Sarcopenia is associated with the Geriatric Nutritional Risk Index in elderly patients with poorly controlled type 2 diabetes mellitus
Shun Matsuura, Koji Shibazaki, Reiko Uchida, Yukiko Imai, Takuya Mukoyama, Shoko Shibata, Hiroshi Morita
Journal of Diabetes Investigation.2022; 13(8): 1366. CrossRef - Increased serum levels of advanced glycation end products are negatively associated with relative muscle strength in patients with type 2 diabetes mellitus
Tsung-Hui Wu, Shiow-Chwen Tsai, Hsuan-Wei Lin, Chiao-Nan Chen, Chii-Min Hwu
BMC Endocrine Disorders.2022;[Epub] CrossRef - Clinical outcomes of multidimensional association of type 2 diabetes mellitus, COVID-19 and sarcopenia: an algorithm and scoping systematic evaluation
Anmar Al-Taie, Oritsetimeyin Arueyingho, Jalal Khoshnaw, Abdul Hafeez
Archives of Physiology and Biochemistry.2022; : 1. CrossRef - Hypoglycaemic therapy in frail older people with type 2 diabetes mellitus—a choice determined by metabolic phenotype
Alan J. Sinclair, Daniel Pennells, Ahmed H. Abdelhafiz
Aging Clinical and Experimental Research.2022; 34(9): 1949. CrossRef - Insulin in Frail, Older People with Type 2 Diabetes—Low Threshold for Therapy
Ahmed Abdelhafiz, Shail Bisht, Iva Kovacevic, Daniel Pennells, Alan Sinclair
Diabetology.2022; 3(2): 369. CrossRef - Sex-Specific Associations Between Low Muscle Mass and Glucose Fluctuations in Patients With Type 2 Diabetes Mellitus
Xiulin Shi, Wenjuan Liu, Lulu Zhang, Fangsen Xiao, Peiying Huang, Bing Yan, Yiping Zhang, Weijuan Su, Qiuhui Jiang, Mingzhu Lin, Wei Liu, Xuejun Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - Lifestyle factors associated with muscle quality in community‐dwelling older people with type 2 diabetes in Japan and Taiwan: a cross‐sectional study
Yuko Yamaguchi, Chieko Greiner, Shu‐Chun Lee, Hirochika Ryuno, Hsin‐Yen Yen, Chiou‐Fen Lin, Ting‐I Lee, Pi‐Hsia Lee
Psychogeriatrics.2022; 22(5): 736. CrossRef - Relationship between Echo Intensity of Vastus Lateralis and Knee Extension Strength in Patients with Type 2 Diabetes Mellitus
Yoshikazu HIRASAWA, Ryosuke MATSUKI, Hideaki TANINA
Physical Therapy Research.2022; 25(3): 113. CrossRef - Time trends (2012–2020) in glycated hemoglobin and adherence to the glycemic targets recommended for elderly patients by the Japan Diabetes Society/Japan Geriatrics Society Joint Committee among memory clinic patients with diabetes mellitus
Taiki Sugimoto, Hisashi Noma, Yujiro Kuroda, Nanae Matsumoto, Kazuaki Uchida, Yoshinobu Kishino, Naoki Saji, Shumpei Niida, Takashi Sakurai
Journal of Diabetes Investigation.2022; 13(12): 2038. CrossRef - Relationship between Diabetes Status and Sarcopenia in Community-Dwelling Older Adults
Kazuhei Nishimoto, Takehiko Doi, Kota Tsutsumimoto, Sho Nakakubo, Satoshi Kurita, Yuto Kiuchi, Hiroyuki Shimada
Journal of the American Medical Directors Association.2022; 23(10): 1718.e7. CrossRef - Low relative hand grip strength is associated with a higher risk for diabetes and impaired fasting glucose among the Korean population
Min Jin Lee, Ah Reum Khang, Dongwon Yi, Yang Ho Kang, Giacomo Pucci
PLOS ONE.2022; 17(10): e0275746. CrossRef - Association between Lower-to-Upper Ratio of Appendicular Skeletal Muscle and Metabolic Syndrome
Hyun Eui Moon, Tae Sic Lee, Tae-Ha Chung
Journal of Clinical Medicine.2022; 11(21): 6309. CrossRef - Association of plasma brain-derived neurotrophic factor levels and frailty in community-dwelling older adults
Eun Roh, Soon Young Hwang, Eyun Song, Min Jeong Park, Hye Jin Yoo, Sei Hyun Baik, Miji Kim, Chang Won Won, Kyung Mook Choi
Scientific Reports.2022;[Epub] CrossRef - Organokines, Sarcopenia, and Metabolic Repercussions: The Vicious Cycle and the Interplay with Exercise
Giulia Minniti, Letícia Maria Pescinini-Salzedas, Guilherme Almeida dos Santos Minniti, Lucas Fornari Laurindo, Sandra Maria Barbalho, Renata Vargas Sinatora, Lance Alan Sloan, Rafael Santos de Argollo Haber, Adriano Cressoni Araújo, Karina Quesada, Jesse
International Journal of Molecular Sciences.2022; 23(21): 13452. CrossRef - Multimorbidity, Frailty and Diabetes in Older People–Identifying Interrelationships and Outcomes
Alan J. Sinclair, Ahmed H. Abdelhafiz
Journal of Personalized Medicine.2022; 12(11): 1911. CrossRef - Determinants of High-Dose Insulin Usage and Upper Extremity Muscle Strength in Adult Patients With Type 2 Diabetes
Eren Imre, Tugce Apaydin, Hatice Gizem Gunhan, Dilek Gogas Yavuz
Canadian Journal of Diabetes.2021; 45(4): 341. CrossRef - Glycemic Control and Insulin Improve Muscle Mass and Gait Speed in Type 2 Diabetes: The MUSCLES-DM Study
Ken Sugimoto, Hiroshi Ikegami, Yasunori Takata, Tomohiro Katsuya, Masahiro Fukuda, Hiroshi Akasaka, Yasuharu Tabara, Haruhiko Osawa, Yoshihisa Hiromine, Hiromi Rakugi
Journal of the American Medical Directors Association.2021; 22(4): 834. CrossRef - A Narrative Review on Sarcopenia in Type 2 Diabetes Mellitus: Prevalence and Associated Factors
Anna Izzo, Elena Massimino, Gabriele Riccardi, Giuseppe Della Pepa
Nutrients.2021; 13(1): 183. CrossRef - Decreased handgrip strength in patients with type 2 diabetes: A cross-sectional study in a tertiary care hospital in north India
Parjeet Kaur, Ritesh Bansal, Bharti Bhargava, Sunil Mishra, Harmandeep Gill, Ambrish Mithal
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(1): 325. CrossRef - Factors associated with relative muscle strength in patients with type 2 diabetes mellitus
Chiao-Nan Chen, Ting-Chung Chen, Shiow-Chwen Tsai, Chii-Min Hwu
Archives of Gerontology and Geriatrics.2021; 95: 104384. CrossRef - Newer anti-diabetic therapies with low hypoglycemic risk-potential advantages for frail older people
Demelza Emmerton, Ahmed Abdelhafiz
Hospital Practice.2021; 49(3): 164. CrossRef - Influence of glucose, insulin fluctuation, and glycosylated hemoglobin on the outcome of sarcopenia in patients with type 2 diabetes mellitus
Yuxi Lin, Yongze Zhang, Ximei Shen, Lingning Huang, Sunjie Yan
Journal of Diabetes and its Complications.2021; 35(6): 107926. CrossRef - Presence and Implications of Sarcopenia in Non-alcoholic Steatohepatitis
Gregory Habig, Christa Smaltz, Dina Halegoua-DeMarzio
Metabolites.2021; 11(4): 242. CrossRef - Sensory-Motor Mechanisms Increasing Falls Risk in Diabetic Peripheral Neuropathy
Neil D. Reeves, Giorgio Orlando, Steven J. Brown
Medicina.2021; 57(5): 457. CrossRef - Impact of frailty metabolic phenotypes on the management of older people with type 2 diabetes mellitus
Ahmed H Abdelhafiz, Demelza Emmerton, Alan J Sinclair
Geriatrics & Gerontology International.2021; 21(8): 614. CrossRef - Type 2 diabetes mellitus in older adults: clinical considerations and management
Srikanth Bellary, Ioannis Kyrou, James E. Brown, Clifford J. Bailey
Nature Reviews Endocrinology.2021; 17(9): 534. CrossRef - Metabolic Syndrome and Sarcopenia
Hiroki Nishikawa, Akira Asai, Shinya Fukunishi, Shuhei Nishiguchi, Kazuhide Higuchi
Nutrients.2021; 13(10): 3519. CrossRef - Angiotensin II inhibition: a potential treatment to slow the progression of sarcopenia
Jeffrey Kingsley, Keiichi Torimoto, Tomoki Hashimoto, Satoru Eguchi
Clinical Science.2021; 135(21): 2503. CrossRef - Muscle strength, an independent determinant of glycemic control in older adults with long-standing type 2 diabetes: a prospective cohort study
Bo Kyung Koo, Seoil Moon, Min Kyong Moon
BMC Geriatrics.2021;[Epub] CrossRef - Associations between homocysteine, inflammatory cytokines and sarcopenia in Chinese older adults with type 2 diabetes
Zhi-Jing Mu, Jun-Ling Fu, Li-Na Sun, Piu Chan, Shuang-Ling Xiu
BMC Geriatrics.2021;[Epub] CrossRef - The Association Between Diabetes Mellitus and Risk of Sarcopenia: Accumulated Evidences From Observational Studies
Yu-Shun Qiao, Yin-He Chai, Hong-Jian Gong, Zhiyessova Zhuldyz, Coen D. A. Stehouwer, Jian-Bo Zhou, Rafael Simó
Frontiers in Endocrinology.2021;[Epub] CrossRef - The utility of the ultrasonographic assessment of the lower leg muscles to evaluate sarcopenia and muscle quality in older adults
Masaaki Isaka, Ken Sugimoto, Taku Fujimoto, Yukiko Yasunobe, Keyu Xie, Yuri Onishi, Shino Yoshida, Toshimasa Takahashi, Hitomi Kurinami, Hiroshi Akasaka, Yasushi Takeya, Koichi Yamamoto, Hiromi Rakugi
JCSM Clinical Reports.2021; 6(2): 53. CrossRef - Associations between grip strength and glycemic control in type 2 diabetes mellitus: an analysis of data from the 2014-2019 Korea National Health and Nutrition Examination Survey
Harim Choe, Hoyong Sung, Geon Hui Kim, On Lee, Hyo Youl Moon, Yeon Soo Kim
Epidemiology and Health.2021; 43: e2021080. CrossRef - Uncontrolled Diabetes as an Associated Factor with Dynapenia in Adults Aged 50 Years or Older: Sex Differences
Clarice Cavalero Nebuloni, Roberta de Oliveira Máximo, Cesar de Oliveira, Tiago da Silva Alexandre, Anne Newman
The Journals of Gerontology: Series A.2020; 75(6): 1191. CrossRef - Identification and prevalence of frailty in diabetes mellitus and association with clinical outcomes: a systematic review protocol
Peter Hanlon, Isabella Fauré, Neave Corcoran, Elaine Butterly, Jim Lewsey, David A McAllister, Frances S Mair
BMJ Open.2020; 10(9): e037476. CrossRef - Longitudinal association of type 2 diabetes and insulin therapy with muscle parameters in the KORA-Age study
Uta Ferrari, Cornelia Then, Marietta Rottenkolber, Canan Selte, Jochen Seissler, Romy Conzade, Birgit Linkohr, Annette Peters, Michael Drey, Barbara Thorand
Acta Diabetologica.2020; 57(9): 1057. CrossRef - Triad of impairment in older people with diabetes-reciprocal relations and clinical implications
A.H. Abdelhafiz, P.C. Davies, A.J. Sinclair
Diabetes Research and Clinical Practice.2020; 161: 108065. CrossRef - Physical activity and exercise: Strategies to manage frailty
Javier Angulo, Mariam El Assar, Alejandro Álvarez-Bustos, Leocadio Rodríguez-Mañas
Redox Biology.2020; 35: 101513. CrossRef - Handgrip measurement as a useful benchmark for locomotive syndrome in patients with type 2 diabetes mellitus: A KAMOGAWA‐DM cohort study
Noriyuki Kitagawa, Takuro Okamura, Nobuko Kitagawa, Yoshitaka Hashimoto, Masahide Hamaguchi, Michiaki Fukui
Journal of Diabetes Investigation.2020; 11(6): 1602. CrossRef - Edmonton frail score is associated with diabetic control in elderly type 2 diabetic subjects
Satilmis Bilgin, Gulali Aktas, Ozge Kurtkulagi, Burcin M. Atak, Tuba T. Duman
Journal of Diabetes & Metabolic Disorders.2020; 19(1): 511. CrossRef - Comparison of field- and laboratory-based estimates of muscle quality index between octogenarians and young older adults: an observational study
Dahan da Cunha Nascimento, Jonato Prestes, Joyce de Sousa Diniz, Pedro Rodrigues Beal, Vicente Paulo Alves, Whitley Stone, Fabiani Lage Rodrigues Beal
Journal of Exercise Rehabilitation.2020; 16(5): 458. CrossRef - Tip 2 Diyabetli Hastalarda Kan Glukoz Seviyesi ile Kas Gücü, Propriosepsiyon ve Vücut Kompozisyonu Arasındaki İlişki
Zahide Betül TAYFUR, Esra ATILGAN
Turkish Journal of Diabetes and Obesity.2020; 4(3): 207. CrossRef - Challenges and Strategies for Diabetes Management in Community-Living Older Adults
Alan J. Sinclair, Ahmed H. Abdelhafiz
Diabetes Spectrum.2020; 33(3): 217. CrossRef - Association between deterioration in muscle strength and peripheral neuropathy in people with diabetes
Tae Jung Oh, Sunyoung Kang, Jie-Eun Lee, Jae Hoon Moon, Sung Hee Choi, Soo Lim, Hak Chul Jang
Journal of Diabetes and its Complications.2019; 33(8): 598. CrossRef - The Association between Body Composition using Dual energy X-ray Absorptiometry and Type-2 Diabetes: A Systematic Review and Meta-Analysis of Observational studies
Preeti Gupta, Carla Lanca, Alfred T. L. Gan, Pauline Soh, Sahil Thakur, Yijin Tao, Neelam Kumari, Ryan E. K. Man, Eva K. Fenwick, Ecosse L. Lamoureux
Scientific Reports.2019;[Epub] CrossRef - MECHANISMS OF ENDOCRINE DISEASE: Sarcopenia in endocrine and non-endocrine disorders
Victoria Zeghbi Cochenski Borba, Tatiana Lemos Costa, Carolina Aguiar Moreira, Cesar Luiz Boguszewski
European Journal of Endocrinology.2019; 180(5): R185. CrossRef - Hyperglycemia induces skeletal muscle atrophy via a WWP1/KLF15 axis
Yu Hirata, Kazuhiro Nomura, Yoko Senga, Yuko Okada, Kenta Kobayashi, Shiki Okamoto, Yasuhiko Minokoshi, Michihiro Imamura, Shin’ichi Takeda, Tetsuya Hosooka, Wataru Ogawa
JCI Insight.2019;[Epub] CrossRef - Hyperglycemia in non‐obese patients with type 2 diabetes is associated with low muscle mass: The Multicenter Study for Clarifying Evidence for Sarcopenia in Patients with Diabetes Mellitus
Ken Sugimoto, Yasuharu Tabara, Hiroshi Ikegami, Yasunori Takata, Kei Kamide, Tome Ikezoe, Eri Kiyoshige, Yukako Makutani, Hiroshi Onuma, Yasuyuki Gondo, Kazunori Ikebe, Noriaki Ichihashi, Tadao Tsuboyama, Fumihiko Matsuda, Katsuhiko Kohara, Mai Kabayama,
Journal of Diabetes Investigation.2019; 10(6): 1471. CrossRef - Diabetic Peripheral Neuropathy as a Risk Factor for Sarcopenia
Tae Jung Oh, Yoojung Song, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 170. CrossRef - Diabetes and frailty
Mariam El Assar, Olga Laosa, Leocadio Rodríguez Mañas
Current Opinion in Clinical Nutrition & Metabolic Care.2019; 22(1): 52. CrossRef - Association of Glucose Fluctuations with Sarcopenia in Older Adults with Type 2 Diabetes Mellitus
Noriko Ogama, Takashi Sakurai, Shuji Kawashima, Takahisa Tanikawa, Haruhiko Tokuda, Shosuke Satake, Hisayuki Miura, Atsuya Shimizu, Manabu Kokubo, Shumpei Niida, Kenji Toba, Hiroyuki Umegaki, Masafumi Kuzuya
Journal of Clinical Medicine.2019; 8(3): 319. CrossRef - Diabetes in the elderly
Ahmed H. Abdelhafiz, Alan J. Sinclair
Medicine.2019; 47(2): 119. CrossRef - Diabetes and Muscle Dysfunction in Older Adults
Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 160. CrossRef - Factors influencing safe glucose-lowering in older adults with type 2 diabetes: A PeRsOn-centred ApproaCh To IndiVidualisEd (PROACTIVE) Glycemic Goals for older people
C.E. Hambling, K. Khunti, X. Cos, J. Wens, L. Martinez, P. Topsever, S. Del Prato, A. Sinclair, G. Schernthaner, G. Rutten, S. Seidu
Primary Care Diabetes.2019; 13(4): 330. CrossRef - Effects of resistance training on neuromuscular parameters in elderly with type 2 diabetes mellitus: A randomized clinical trial
Cíntia E. Botton, Daniel Umpierre, Anderson Rech, Lucinéia O. Pfeifer, Carlos L.F. Machado, Juliana L. Teodoro, Alexandre S. Dias, Ronei S. Pinto
Experimental Gerontology.2018; 113: 141. CrossRef - Management of Elderly Diabetes Patients Who Are Unable to Self-Care
Bok Rye Song
The Journal of Korean Diabetes.2018; 19(4): 232. CrossRef - Decreased Muscle Strength and Quality in Diabetes-Related Dementia
Akito Tsugawa, Yusuke Ogawa, Naoto Takenoshita, Yoshitsugu Kaneko, Hirokuni Hatanaka, Eriko Jaime, Raita Fukasawa, Haruo Hanyu
Dementia and Geriatric Cognitive Disorders Extra.2017; 7(3): 454. CrossRef - Diabetes and Sarcopenia
Dong Hyun Kim, Tae Yang Yu
The Journal of Korean Diabetes.2017; 18(4): 239. CrossRef - Frailty and sarcopenia - newly emerging and high impact complications of diabetes
Alan J. Sinclair, Ahmed H. Abdelhafiz, Leocadio Rodríguez-Mañas
Journal of Diabetes and its Complications.2017; 31(9): 1465. CrossRef - Association of diabetic retinopathy with both sarcopenia and muscle quality in patients with type 2 diabetes: a cross-sectional study
Tatsuya Fukuda, Ryotaro Bouchi, Takato Takeuchi, Yujiro Nakano, Masanori Murakami, Isao Minami, Hajime Izumiyama, Koshi Hashimoto, Takanobu Yoshimoto, Yoshihiro Ogawa
BMJ Open Diabetes Research & Care.2017; 5(1): e000404. CrossRef - Practical considerations for managing patients with diabetes and dementia
Michelle L Mair, Rohin Athavale, Ahmed H Abdelhafiz
Expert Review of Endocrinology & Metabolism.2017; 12(6): 429. CrossRef - Sarcopenia: An Endocrine Disorder?
Alexis McKee, John E. Morley, Alvin M. Matsumoto, Aaron Vinik
Endocrine Practice.2017; 23(9): 1143. CrossRef - Response: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (Diabetes Metab J 2016;40:140-6)
Ji Won Yoon, Hak Chul Jang
Diabetes & Metabolism Journal.2016; 40(3): 250. CrossRef - Salivary lactate dehydrogenase and aminotransferases in diabetic patients
Barbara Malicka, Katarzyna Skoskiewicz-Malinowska, Urszula Kaczmarek
Medicine.2016; 95(47): e5211. CrossRef - Explanatory models of muscle performance in acromegaly patients evaluated by knee isokinetic dynamometry: Implications for rehabilitation
Agnaldo José Lopes, Arthur Sá Ferreira, Evelyn Mendes Walchan, Mauricio Santos Soares, Priscila Santos Bunn, Fernando Silva Guimarães
Human Movement Science.2016; 49: 160. CrossRef - Letter: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (Diabetes Metab J 2016;40:140-6)
Jun Sung Moon
Diabetes & Metabolism Journal.2016; 40(3): 248. CrossRef - Sarcopenia, Frailty, and Diabetes in Older Adults
Hak Chul Jang
Diabetes & Metabolism Journal.2016; 40(3): 182. CrossRef
- Downhill running and caloric restriction attenuate insulin resistance associated skeletal muscle atrophy via the promotion of M2-like macrophages through TRIB3-AKT pathway
- Clinical Care/Education
- Clinical Characteristics and Metabolic Predictors of Rapid Responders to Dipeptidyl Peptidase-4 Inhibitor as an Add-on Therapy to Sulfonylurea and Metformin
- Ye An Kim, Won Sang Yoo, Eun Shil Hong, Eu Jeong Ku, Kyeong Seon Park, Soo Lim, Young Min Cho, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi
- Diabetes Metab J. 2015;39(6):489-497. Published online November 27, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.6.489
- 3,502 View
- 39 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase-4 (DPP-4) inhibitor add-on therapy is a new option for patients with inadequately controlled type 2 diabetes who are taking combined metformin and sulfonylurea (SU). We evaluated the efficacy and safety of this triple therapy and the characteristics of rapid responders and hypoglycemia-prone patients.
Methods We included 807 patients with type 2 diabetes who were prescribed a newly added DPP-4 inhibitor to ongoing metformin and SU in 2009 to 2011. Glycemia and other metabolic parameters at baseline, 12, 24, and 52 weeks, as well as episodes of hypoglycemia were analyzed. Rapid responders were defined as patients with ≥25% reduction in glycosylated hemoglobin (HbA1c) within 12 weeks.
Results At baseline, while on the submaximal metformin and SU combination, the mean HbA1c level was 8.4%. Twelve weeks after initiation of DPP-4 inhibitor add-on, 269 patients (34.4%) achieved an HbA1c level ≤7%. Sixty-six patients (8.2%, 47 men) were rapid responders. The duration of diabetes was shorter in rapid responders, and their baseline fasting plasma glucose (FPG), HbA1c, C-peptide, and homeostasis model assessment of insulin resistance were significantly higher. Patients who experienced hypoglycemia after taking DPP-4 inhibitor add-on were more likely to be female, to have a lower body weight and lower triglyceride and FPG levels, and to have higher homeostasis model assessment of β-cells.
Conclusion An oral hypoglycemic triple agent combination including a DPP-4 inhibitor was effective in patients with uncontrolled diabetes. Proactive dose reduction of SU should be considered when a DPP-4 inhibitor is added for rapid responders and hypoglycemia-prone patients.
-
Citations
Citations to this article as recorded by- A genetic variant in GLP1R is associated with response to DPP-4 inhibitors in patients with type 2 diabetes
Eugene Han, Hye Sun Park, Obin Kwon, Eun Yeong Choe, Hye Jin Wang, Yong-ho Lee, Sang-Hak Lee, Chul Hoon Kim, Lee-Kyung Kim, Soo Heon Kwak, Kyong Soo Park, Chul Sik Kim, Eun Seok Kang
Medicine.2016; 95(44): e5155. CrossRef
- A genetic variant in GLP1R is associated with response to DPP-4 inhibitors in patients with type 2 diabetes

 KDA
KDA
 First
First Prev
Prev





